A Guide to Using Prebuilt Modules to Launch a Health App
You can tell when a health app idea is starting to get real, because the first slide that shows up in the deck is some version of: “We’ll move fast by using prebuilt modules.”
On paper, it sounds like the perfect cheat code. Why reinvent auth, scheduling, telehealth, or an EMR-lite when someone else has already done the hard, boring, HIPAA-flavored work? Just grab a few building blocks, wire them together, and boom: virtual clinic in a quarter.
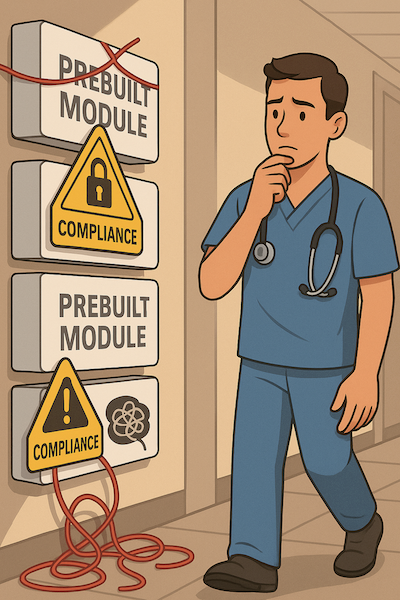
Except that’s not how it usually plays out. In practice, founders end up stuck between two bad extremes:
- rebuilding basic plumbing from scratch because “we’re special,” or
- bending their entire care model around a stack of generic components that were never designed for their specialty, their workflows, or their risk profile.
This guide is for the middle path.
We’ll break down what “prebuilt modules” actually mean in healthcare (beyond marketing decks), when they’re a gift and when they’re an anchor, which building blocks almost every app should reuse, and how to avoid painting yourself into a corner with lock-in, integration debt, and roadmap roulette.
And yes, we’ll talk about where platforms like Specode fit into that picture — not as “AI magic,” but as a way to stand up the boring 70–80% quickly, without sacrificing ownership of the 20–30% that actually makes your product worth building.
Key Takeaways
- Don’t start with “modules vs custom,” start with fit. If 70–80% of your app looks like standard care flows, reuse building blocks; reserve custom engineering for the 20–30% that’s truly clinical-critical, differentiating, and fast-changing.
- You’re not picking features, you’re picking constraints. Before committing to any prebuilt stack, run it through a grown-up checklist: exit path (data + code), integration model, roadmap discipline, and “module mesh” risk. If you can’t explain where truth lives and how it moves, don’t ship on it.
- Treat Specode as rails, not a cage. Specode’s AI builder stitches HIPAA-ready components (auth, portals, intake, EMR-lite, telehealth, notifications, commerce, tracking, and more) into real clinical workflows, then hands you a codebase you own — so your team (or ours) can layer on AI agents, deep EHR integrations, and specialty-grade logic without ever starting from zero.
What “Prebuilt Modules” Actually Mean in Healthcare
Let’s start by killing the fantasy: “prebuilt modules” are not magic Lego blocks you click together over a weekend and somehow get a compliant virtual clinic. In healthcare, a “module” usually means, “someone else already did the boring, painful part… but you still have to wire it into your very specific version of reality.”

When most generic low-code tools mention “prebuilt components or modules,” they’re talking about UI widgets and CRUD views: tables, forms, dashboards. Helpful, but that’s not a care pathway. Healthcare modules look more like this:
UX Modules
Think patient portals and provider workspaces:
- Patient portal: appointments, visit history, secure messages, tasks.
- Provider dashboard: schedule, chart inbox, work queues, documentation views.
If a platform can’t give you at least this much out of the box, you’re not buying modules, you’re buying a design project.
Workflow Modules
This is where it gets closer to how care actually happens:
- Intake and triage flows.
- Virtual visit workflows (pre-visit, in-visit, post-visit).
- Follow-up plans, refills, billing, care coordination.
Good workflow modules encode opinionated defaults: “this is roughly how a telepsych visit or a PT follow-up works.” Your job is to decide if those opinions match your clinic or if you’ll spend months fighting them.
Infrastructure Modules
This is the plumbing nobody wants to rebuild:
- Auth, roles, and SSO.
- PHI storage, encryption, audit logging.
- EHR / FHIR connectors, eRx, labs, notification engines.
These modules don’t usually have pretty UIs; they’re about not waking up to a security incident or a broken EHR feed.
Now layer on the uncomfortable truth: every platform that markets “prebuilt modules” — blueEHR, blueConsole, Mahalo, pick your flavor — is really selling opinionated starting points. You still configure, integrate, and, in many cases, write real code around them. The marketing deck skips that part.
So for this guide, when we say “prebuilt modules or components,” we’re not talking about drag-and-drop toys. We’re talking about healthcare-specific UX, workflow, and infrastructure components with assumptions baked in: which roles exist, which fields are required, how an encounter is stored, what an “appointment” even means.
The rest of the article is about using those assumptions in your favor — and knowing exactly when to push back, extend them, or replace them before they quietly become your biggest constraint.
When Prebuilt Modules Are a Good Fit and When You Should Walk Away
Here’s the uncomfortable truth about prebuilt healthcare modules (or components, or building blocks—at Specode we tend to say components): they’re either an accelerator or an anchor. The trick is knowing which one you’re buying before you wire half your care model into them.
Great Fit When…
Prebuilt modules shine when your app looks like a recognizable clinic, just with your twist on top:
- You’re building standard-ish flows: virtual-first primary care, group therapy, coaching platforms, RPM programs, ePharmacy storefronts, or simple specialty clinics where visits still follow a familiar pattern (e.g., primary care telehealth, standard ortho follow-ups, CBT-based mental health programs).
- You need to ship an MVP/V1 in months, not years, and your differentiation lives in workflow tuning, content, or experience — not in hand-coding authentication or building a scheduling engine from scratch.
- Your integration needs are “reasonable”: one primary EHR or a lightweight EMR, a single payments provider, maybe 1–2 devices and straightforward labs.
- Your regulatory footprint is mostly HIPAA and payer compliance; you’re not, on day one, trying to clear a software-as-medical-device workflow through an FDA reviewer who will ask why every screen behaves the way it does.
In that world, prebuilt components give you a sane starting point: standard care rails you can bend a bit, not raw steel you have to forge.
Bad or Risky Fit When…
On the other end of the spectrum, a “module-first” approach can quietly sabotage you:
- You’re building safety-critical, device-grade software where every screen and transition has to map to a specific IEC 62304 / FDA strategy and risk file. Here, any hidden behavior inside a black-box module becomes your problem during audit.
- You’re inventing a new category with very non-standard workflows: complex multi-party marketplaces, unusual longitudinal care models, novel data visualizations that don’t look like “encounter + note.” Trying to squeeze that into a generic care-pathway component is how you end up with a Frankenstack.
- You’re in a specialty where the “generic clinic” flow is actively harmful or wildly inefficient if forced: nuanced oncology pathways, high-acuity perioperative workflows, fertility rules that blow up standard intake and consent, etc.
- You already know you’ll need deep EHR orchestration across multiple systems with custom mappings, cross-organization data sharing, and gnarly edge cases from day one. Plug-and-play connectors are rarely plug-and-play at that level.
Plug-and-play connectors are rarely plug-and-play at that level. If you’re tempted by the idea of a plug-and-play health app, this breakdown walks through what it actually takes to make one safe, compliant, and maintainable in the real world.
In these cases, prebuilt modules can still help with plumbing (auth, logging, notifications), but letting them dictate your core workflow is asking for regrets.
Rules of Thumb
When you’re staring at a menu of prebuilt healthcare components, a few simple heuristics help:
- If ≥70% of what you need looks like standard modules (portals, intake, telehealth, basic EMR, payments) → a module-first or component-first strategy is worth serious consideration.
- If <50% overlap and you anticipate heavy regulation or highly idiosyncratic specialty workflows → bias toward custom, and use prebuilt blocks only for infrastructure pieces.
Then apply a simple “component maturity” lens:
- Commodity, stable, non-differentiating capabilities (auth, audit, generic messaging, basic notifications) → reuse as prebuilt modules/components for as long as possible.
- High-differentiation, specialty-specific workflows or rapidly evolving logic (clinical decision rules, niche scheduling rules, risk scores, proprietary triage) → plan to customize early, or treat prebuilt modules as a temporary scaffold you’ll later “extract” into your own implementation.
That’s the real game: not “prebuilt vs custom,” but knowing which 20–30% of your product should never be trapped inside someone else’s idea of a module.
The Core Modules Most Health Apps Reuse
If you strip away everyone’s pitch decks, most healthcare apps are built from the same 6–7 prebuilt building blocks. The difference between “we launched in 4 months” and “we’ve been in dev for 18 months” is usually whether you rebuilt this plumbing from scratch or stood on someone else’s shoulders.

The goal here: name the usual suspects and give you a quick lens for what to look for in each prebuilt component category.
Authentication and Roles
This is the gatekeeper layer. If you get it wrong, nothing else matters. A solid auth/roles component should give you:
- Secure login, MFA-ready, patient/provider/admin roles, SSO options (OIDC/SAML).
- PHI-safe sessions and strong audit trails for login attempts, role changes, and permission escalations.
The non-negotiables for prebuilt auth modules:
- First-class audit logging on auth and privilege changes.
- The ability to represent unusual roles: care coordinators, supervisors, billing-only users, external referring providers, even “read-only auditor” accounts.
Specialty nuance: ask yourself how easily you can model roles for multi-location dental groups, multi-clinic mental health practices, or fertility clinics where lab, clinical, and financial teams all need different slices of the truth.
Patient and Provider Portals
Portals are where your app either feels “clinic-grade” or like a side project. Typical prebuilt portal components should cover:
- Patient dashboards: appointments, records, messaging, tasks, sometimes bills and care plans.
- Provider dashboards: schedule, chart inbox, work queues, documentation views, and quick actions.
Things to check when evaluating these modules:
- Multi-tenant support (can you run multiple organizations on one stack?).
- Branding flexibility and white-labelability — can you really make it look like your brand?
- Performance at scale: does it still feel snappy with real-world data volumes and provider rosters?
Watch how much you can adjust navigation, terminology, and views to match specialty workflows: therapy session notes vs SOAP notes vs orthodontic treatment plans should not feel like the same template with different labels hacked on top.
Scheduling, Telehealth, and Communication
This is the “patient shows up and talks to someone” layer of your prebuilt component stack. At minimum, you’re looking for:
- Appointment booking, provider availability, and reminders.
- Video visits with secure, healthcare-friendly defaults.
- Chat/secure messaging and, ideally, support for group sessions.
Questions to interrogate every prebuilt scheduling/telehealth module with:
- Is telehealth native or bolted on via a third-party widget?
- How does it log clinical context into encounters or notes — or does it just show “Video call happened”?
- Can it handle specialty patterns: recurring therapy sessions, multi-resource bookings for procedure rooms, lab + consult combos, or multidisciplinary visits?
Intake, Surveys, and e-Consent
This is where a lot of “simple” prebuilt modules go to die once real clinicians get involved. A credible intake/survey component should support:
- PROs and questionnaires.
- Dynamic intake flows and structured assessments.
- e-Consent with proper tracking and versioning.
Things to watch for:
- Language support and localization.
- Branching logic and conditional flows that don’t require a PhD in config.
- Re-usable forms across locations and programs.
- Export formats: PDFs for humans, FHIR resources (or similar) for machines.
Specialty nuance: can the data model stretch to handle longer psych intake flows, detailed reproductive histories in fertility, dentistry-specific histories — or are you going to end up hacking all of that into generic “other notes” fields?
Clinical Data and EMR Lite
Most prebuilt healthcare platforms quietly ship a “mini-EMR” whether they admit it or not. Expect at least:
- Problems, meds, allergies, encounters, notes, and tasking.
- Basic care plans and activity tracking.
Integration patterns usually fall into two buckets:
- An embedded “EMR-lite” that wants to be your primary system of record.
- Connectors to external EHRs (FHIR APIs, Momentum-style integration modules) where the app is more of a smart layer on top.
Your job is to decide whether this EMR-lite is actually good enough for your specialty or just a staging area before data moves into the real system of record. If it’s the latter, you want very clear, well-documented sync semantics.
Payments, Commerce, and Rewards
Payments are where your prebuilt stack meets Planet Reality. Good payments/commerce components typically include:
- E-commerce for meds/OTC and services.
- Billing, invoices, and subscription plans.
- Self-pay flows and, sometimes, basic insurance support.
- Adherence or engagement rewards (points, credits, discounts).
Consider whether the module can handle mixed business models: cash-pay mental health + insurance panels, memberships for coaching programs, bundled procedures, or hybrid online/offline services.
Notifications, Content and Outcomes Tracking
Finally, you have the “keep people engaged and out of the ER” layer. Typical prebuilt components here cover:
- Multi-channel nudge engines (email/SMS/push).
- Education libraries and content delivery.
- Symptom, mood, or vitals tracking tied to visits or programs.
What to check:
- Routing rules by specialty: escalation rules in behavioral health should not look like dermatology.
- Throttling and safety controls so you don’t spam patients or providers.
- Whether you can tie notifications and content to outcomes, visit types, and specific cohorts, not just “blast campaign X to list Y.”
If you get these seven categories roughly right with prebuilt modules or components, you’ve covered 70–80% of the plumbing most health apps quietly share — and bought yourself time to focus on the weird, valuable 20% that actually sets you apart.
What Prebuilt Components Specode Actually Ships
At this point it’s fair to ask: “OK, but what does a ‘component-first’ stack actually look like in the real world?” In Specode’s case, the answer is: most of the categories you’ve just read about come prewired as healthcare-native components, not generic widgets.
- On the access and identity side, you get authentication and session management out of the box: secure email/password login, MFA-ready hooks, and unified access for patients, providers, and admins, with role-based permissions layered on top.
- For patient and provider experience, Specode ships patient dashboards and profiles, provider dashboards and profiles, plus provider search and availability components: think “find a clinician → see their profile → book a slot” as a reusable pattern, not a one-off build.
- The care-journey layer is covered by intake form components (branching questionnaires, visit context, medical history), scheduling and live calendars, and a basic EMR: problems, meds, allergies, encounters, SOAP notes, and an immutable audit trail that can either stand alone or sit alongside a system like Canvas Medical.
- On the care delivery front, there are telehealth components (secure video visits with waiting room and in-session chat) plus HIPAA-ready chat/video modules for 1:1 or group communication, wired into scheduling and the EMR-lite so visits aren’t just “Zoom links with vibes.”
- The engagement and education layer shows up as notifications (in-app, email, SMS, push, with preferences and escalation rules) and a resources component—a mini CMS for education content and after-visit materials.
- For commerce, Specode includes a product catalog, cart, and a healthcare-aware checkout flow that can collect demographics and medical context, plus outcome/engagement components: symptom trackers, mood journals, vitals dashboards, and goal tracking.
Above all of this sits the AI assistant, which doesn’t just generate screens but assembles these components into working flows—so you’re not prompting for “a telehealth app,” you’re effectively asking for “this combination of scheduling, intake, EMR-lite, telehealth, notifications, and tracking wired together in a HIPAA-safe way.”
When you outgrow the defaults, you can still extend or replace individual components without tearing the whole thing down.
Four Ways Teams Use Prebuilt Modules to Ship Faster
Once you accept that most health apps are stitched together from prebuilt building blocks, the next question is: which kind of stack are you actually signing up for? From what we’ve seen in the wild, most teams fall into one of four patterns — and each one comes with its own speed boosts and hangovers.
Pattern 1: Pure No-Code App Builders
This is the “get me something on screen by Friday” option. Think generic no-code platforms with healthcare-ish templates: drag-and-drop UI, prebuilt screens, basic workflows.
Why founders love it:
- Fastest visible progress: you can click your way to a demo in days.
- Non-technical teams can own a lot of the changes.
- Cheap to start, especially for early validation.
The fine print:
- You’re renting someone else’s data model and logic; deep customization is usually “possible” in the same way climbing Everest is “walkable.”
- Integrations tend to be shallow: good for “send data to X,” painful for “X is my system of record.”
- When your care model evolves, you discover the prebuilt modules are welded to the platform, not your roadmap. Migration often means a partial rebuild.
Use this when you’re still figuring out what you’re building. Don’t plan your long-term architecture around it.
If you want a clearer picture of how low-code and no-code platforms actually perform in real healthcare use cases — strengths, limitations, and where teams get blindsided — this guide on low-code and no-code platforms for health app development breaks it down with examples and architecture-level detail.
Pattern 2: Healthcare-Specific Modular Platforms
These are the opinionated SaaS platforms that ship a buffet of prebuilt healthcare modules: scheduling, telehealth, intake, EMR-lite, messaging, billing, sometimes RPM. You compose an app from their catalog of components and configuration panels.
Why it’s attractive:
- You get healthcare-aware building blocks: CPT/ICD codes, encounters, secure messaging, all wired together.
- Hosting, security, and updates are handled; you ride their releases.
- Great if your clinic looks a lot like their “model customer.”
Where teams get burned:
- The more modules you enable, the more you’re living inside their operating system. Your differentiation risks becoming “we configured the same platform slightly differently.”
- Deep specialty workflows often expose the limits of toggle-based customization.
- Exiting later means extracting data, rebuilding workflows, and re-implementing integrations you thought were “prebuilt forever.”
This works well for organizations that want a modern clinical system with modest customization — less so for founders chasing a new category.
Pattern 3: Integration & Backend Frameworks
Here the focus isn’t shiny UI modules; it’s backend building blocks: auth, FHIR APIs, EHR connectors, queues, job runners. You assemble your own experiences on top of a healthcare-grade foundation.
The upside:
- Strong primitives for identity, PHI storage, and interoperability.
- You keep control of UX, workflows, and data models at the application layer.
- Better fit for teams with in-house engineers who want to own the product’s “feel” but don’t want to reinvent security and integrations.
The trade-offs:
- Time to first demo is slower than pure no-code or turnkey modular platforms.
- You’re taking on real engineering work; founders without a technical partner can get stuck.
- Misuse the primitives and you can still end up with a module-mesh: five systems, ten interfaces, unclear system of record.
This pattern is ideal if your main headache is “talk to Epic/Cerner/whatever, safely,” and you’re ready to design your own front-end experience.
If you’re in that camp and need a more concrete playbook, this EHR integration guide walks through architectures, trade-offs, and the gotchas teams hit when wiring real-world EHRs into modern health apps.
Pattern 4: AI-Assisted Component Assembly with Code Ownership (Specode)
The fourth pattern tries to split the difference: use healthcare-native components (auth, portals, intake, EMR-lite, telehealth, notifications, commerce, tracking), but assemble them with an AI assistant — and keep the code.
In practice, that looks like:
- You describe the clinic you’re building — who the users are, how visits work, what needs to be tracked — and the AI composes flows from prebuilt components instead of hallucinating from scratch.
- You get a working health app with sane defaults for HIPAA, audit trails, and data models, plus a real codebase engineers can extend.
- As certain flows become strategic (your triage logic, your care programs, your dashboards), you can progressively replace or deepen those pieces without ripping out the whole stack.
The promise here isn’t “AI builds your app in one prompt.” It’s: prebuilt healthcare components + AI to assemble them + an escape hatch when you need something the components were never designed for. That escape hatch — code ownership and extensibility — is what separates a fast start from a future rewrite.
Things to Be Cautious About When Building on Prebuilt Modules
Prebuilt healthcare modules are like hospital coffee: better than nothing, but you really need to check what’s in the cup before you start relying on it every day. The promise is real — faster launches, less boilerplate, fewer infrastructure mistakes — but there are a few ways these building blocks can quietly turn into handcuffs.
Let’s talk about where teams get burned.
Hidden Lock-In and Limited Extensibility
The biggest risk isn’t “this platform is bad,” it’s “this platform is fine… and now we can’t leave.”
Common patterns:
- Data lives in a proprietary schema you can’t easily export or re-host.
- “Custom logic” means scripting in a platform-specific language that doesn’t exist anywhere else.
- The only way to do something important is via config UIs that don’t translate into real code.
If your core workflows, pricing logic, or clinical rules only exist as checkboxes and mystery scripts inside someone else’s prebuilt components, you don’t have an app — you have a very elaborate settings file.
Ask early: What does “exiting” this stack look like in 3–5 years? If the honest answer is “a rewrite,” treat lock-in as a cost, not a footnote.
Compliance Assumptions
“HIPAA compliant” is a marketing phrase. Compliance is an architecture.
Prewired modules can give you a head start — encryption, PHI storage, audit logging, BAAs — but they rarely cover your whole risk surface:
- Does every building block produce logs your compliance officer can actually use?
- Are BAAs in place for all the services involved (video, SMS, storage, analytics)?
- Where exactly does PHI cross boundaries between modules and vendors?
Integration-heavy setups (EHR, labs, payments) still need a real review: data flows, logging, access control. If a vendor waves their SOC 2 or HIPAA badge and tells you “it’s all handled,” that’s your cue to start asking detailed questions.
Workflow Mismatch and Clinician Burnout
Prebuilt flows are opinionated. That’s the point. But if those opinions don’t match how your clinicians actually practice, you’ll pay for it in workarounds and resentment.
Red flags:
- Nurses keeping parallel spreadsheets because “the app doesn’t match how we round.”
- Therapists writing real notes in Word and pasting summaries into the platform.
- Physicians clicking through three extra screens “because the module wants it that way.”
It’s worse in nuanced specialties: oncology, perioperative care, fertility, complex behavioral health. If you have to contort your care model to satisfy a generic scheduling or documentation component, the module is winning and your clinic is losing.
Performance and Scalability Gotchas
A lot of prebuilt stacks are optimized for demos and pilots, not for “thousands of patients across dozens of sites.”
Watch for:
- Shared multi-tenant backends where your performance depends on your noisiest neighbor.
- Hard, poorly documented limits on API calls, messages, or concurrent sessions.
- Reporting or analytics that fall over once you hit real-world data volumes.
It’s fine if the first version is a little scrappy. It’s not fine if “adding another state” requires a database migration and a performance war room.
Cost Creep
Almost every platform looks affordable in the first month. The real cost shows up once you have usage.
Common sources of surprise:
- Per-user or per-provider pricing that scales faster than your revenue.
- Premium add-ons for “advanced” features that are actually table stakes (notifications, eRx, extra environments).
- Consulting or “success” packages you end up buying just to work around built-in limitations.
Run a 3–5 year TCO scenario: best case, expected, worst case. If the worst case looks like “rebuild from scratch because the economics broke,” you want to know that before Go-Live day.
Roadmaps, Breaking Changes, and Frozen Stacks
One more thing people rarely ask when they buy into prebuilt components: is this stack going to move with you, or move without you? Two equal and opposite risks:
- The roadmap is too aggressive: new versions of modules ship fast, and with them come breaking changes in data models, APIs, or UI flows. Suddenly your carefully tuned clinic workflow is living on top of a moving floor.
- The roadmap is nonexistent: the catalog looks fine today, but there’s no credible plan for new building blocks you’ll need in year two — new visit types, programs, or integrations – so you end up bolting on a second platform next to the first.
At minimum, you want to see:
- A public (or at least transparent) roadmap for major modules and upcoming components.
- Clear versioning and deprecation policies: how long old versions live, how migrations are handled, who does the work.
- A story for how changes are communicated and tested before they hit your production workflows.
If a vendor can’t show you where their building blocks are headed, you’re not just buying today’s modules — you’re betting your roadmap on theirs, blind.
The “Module Mesh” Problem (Integration Debt at Scale)
This is the one that sneaks up on teams. You start with a few prebuilt services: auth, telehealth, EMR-lite, notifications, payments. Each looks clean in isolation. Then you connect them.
With five systems, you don’t have five relationships — you might have ten or fifteen:
- Mapping users and roles between identity, EHR, and messaging.
- Syncing appointments between scheduling, telehealth, and calendars.
- Threading clinical context through chat, video, and documentation.
Each vendor ships updates on its own schedule. One small schema change or API tweak can silently break a downstream workflow. Debugging becomes a sport where nobody fully owns the end-to-end journey.
Mitigations:
- Keep the number of “systems of record” as small as humanly possible.
- Centralize identity and events instead of letting every component invent its own truth.
- Favor platforms that offer a coherent integration layer over a pile of point-to-point connectors.
Prebuilt modules and components can give you a real unfair advantage — but only if you treat them as part of an architecture, not a shopping cart. Go in with a lock-in plan, a compliance story, and a clear idea of how you’ll keep the mesh from turning into a knot.
Evaluation Checklist – Choosing the Right Module Stack for Your App
This is the part you can literally keep open in another tab while you’re on a vendor demo. You’re not just buying prebuilt modules; you’re buying a set of constraints. The goal here is to make those constraints visible before you sign anything.
Think of this as a quick due-diligence grid for any prebuilt component stack or health app platform.
1. Compliance & Security
Ask: “If something goes wrong, can we prove we did the right thing?”
- Do they sign a BAA themselves, or only via partners?
- Is audit logging deep enough to reconstruct who saw/changed what, and when?
- How is PHI stored and encrypted (at rest, in transit, backups, logs)?
- Can you choose data residency (region/tenant isolation), or is it “one big bucket for everyone”?
Red flag: they lead with a certification logo, not with a clear architecture story.
2. Data & Integration Model
Ask: “Where does the truth live, and how does it move?”
- Do they support FHIR or other standard models, or is everything trapped in proprietary schemas?
- How do integrations work: native connectors, custom work each time, or “talk to our partner”?
- Can the same patient, encounter, and appointment IDs flow cleanly across auth, EMR, telehealth, messaging, and payments?
- Is there a single event stream / webhook model, or five different notification mechanisms you have to babysit?
Red flag: you hear “we integrate with everything” and zero detail about how and who owns what once it’s wired up.
3. Extensibility & Ownership
Ask: “What happens when we outgrow the defaults?”
- Can you export code or at least export your data in a sane, re-importable form?
- Is there a documented way to inject your own services, logic, or UIs into their flows?
- Can your devs extend components using mainstream tech, or only via proprietary scripting?
- If the company disappeared tomorrow, how much of your stack would still be under your control?
Red flag: roadmap answers are great, but there’s no concrete mechanism to bend or replace individual building blocks.
4. Workflow Fit
Ask: “Does this actually match how our clinicians work on Tuesday at 3 p.m.?”
- Can you rename fields, steps, and entities to match your specialty’s language?
- How hard is it to change the order of steps in a visit, care program, or intake flow?
- Can different locations or service lines run slightly different workflows without creating a second app?
- Have real clinicians from your specialty tried to map their current day into these flows?
Red flag: the demo looks great, but every “can we change…?” question gets “not yet, but we can add it to the roadmap.”
5. Total Cost of Ownership (3–5 Years)
Ask: “What does this actually cost once we’re successful?”
- Pricing basis: per user, per provider, per message, per visit, per environment?
- Extra fees for: additional environments, higher API throughput, premium integrations, analytics, support tiers?
- What happens if your usage doubles or triples — does pricing grow linearly, or in steps?
- How much “professional services” effort is usually needed to go from config to production for a customer like you?
Red flag: they’re happy to talk about pilot pricing, vague about what a large customer is actually paying.
6. Roadmap & Support
Ask: “Is this platform evolving with us, or evolving at us?”
- Is there a visible roadmap for major modules and new components (even if high-level)?
- How are breaking changes handled: versioning, deprecation windows, migration tooling?
- How do you test upcoming changes: sandboxes, release notes, explicit change logs?
- What does support look like when something critical breaks in your live workflows?
Red flag: you hear “we ship fast” and nothing about how they keep existing customers stable while doing it.
7. Component Maturity Matrix (Sanity Check Before You Commit)
Last step: run your own components through a simple lens before locking in any stack. For each major building block (auth, portals, intake, EMR-lite, telehealth, notifications, commerce, etc.), score it on three axes:
- Clinical criticality – Does this touch diagnosis/therapy, or mostly admin/ops?
- Differentiation – Is this your secret sauce, or commodity plumbing?
- Change velocity – Is this logic relatively stable, or are you going to tweak it every quarter?
Then:
- High criticality + high differentiation + high change velocity → lean toward custom (or treat prebuilt as a short-term scaffold you plan to replace).
- Low differentiation + low-to-medium change velocity → strong candidates for long-term use of prebuilt modules/components.
If you can’t explain, in one slide, which parts of your app live in prebuilt building blocks and which will eventually be “yours,” you’re not choosing a module stack — you’re gambling on it.
How to Phase Your Build: Start with Modules, Then Layer in Custom
The worst way to use prebuilt healthcare building blocks is “all or nothing”: either you try to do everything in generic modules, or you swear them off and hand-roll auth in 2025. The sane path lives in the middle: use prebuilt components to stand up the boring 70–80%, then gradually pull your “secret sauce” out into real, owned code.

Think of it as a roadmap, not a one-time decision.
Phase 1: Clarify the 20% That Makes You Different
Before you touch any platform:
- Write down the few workflows that actually define you: your care model, triage logic, programs, dashboards, outcomes.
- Separate those from things nobody brags about (“we have login and appointment reminders”).
- Run them through your internal version of the component maturity matrix: high criticality + high differentiation + fast-changing = “do not entomb this inside someone else’s config forever.”
You don’t need a 100-page PRD. You need a ruthless list of “this must eventually be ours.”
If you need a broader blueprint before you even pick components — from scoping and team structure to timelines and risks — this healthcare app development guide lays out the full journey end to end.
Phase 2: Assemble the 80% with Prebuilt Components
Now you let modules do what they’re good at:
- Stand up auth, roles, patient/provider portals, intake, scheduling, telehealth, notifications, basic EMR-lite, and payments using prebuilt building blocks.
- Keep your domain logic thin at this stage; treat this as scaffolding to prove flows, not the final shape of your product.
- Make one architectural decision early: centralize identity and events (who did what, when). Everything else hangs off that spine.
Goal of this phase isn’t “perfect.” It’s “safe, demo-able, and good enough for a controlled pilot.”
Phase 3: Integrate Your Core Systems
Once the base experience works, plug it into the real world:
- Wire in EHR, labs, devices, and external services using integration components or frameworks.
- Decide explicitly what each system is the source of truth for (patients, encounters, billing, consents, etc.).
- Put guardrails around your stack so you don’t drift into module-mesh chaos: consistent IDs, a single event bus or integration layer, and clear ownership of each interface.
If this phase feels messy, that’s normal. The mistake is letting “temporary sync scripts” quietly become permanent architecture.
There’s a surprisingly small set of components and infrastructure choices that keep early teams from drifting into integration chaos — the leanest stack patterns are outlined here if you want a blueprint before wiring in your real systems.
Phase 4: Customize Around Your “Secret Sauce” (Extraction Pattern)
This is where you start earning your valuation.
Pick the 1–2 flows that matter most (e.g., triage, onboarding, program management, analytics) and apply the extraction pattern:
- Shadow the generic component with your own: new screens, services, or APIs that sit beside the prebuilt flow.
- Shift logic gradually: move branching, rules, and calculations into your own services, while the component still handles basics (identity, storage, notifications).
- Narrow the old module’s role: maybe it still sends messages or handles payments, but it no longer defines how care flows.
You’re not “ripping out” modules; you’re demoting them from “brain” to “infrastructure.” Done right, users barely notice the transition. Internally, you go from configuration to real IP.
Phase 5: Harden for Scale and Audits
Once you’ve proven the model and extracted the important parts:
- Load-test the whole pipeline: logins → intake → visits → documentation → billing → reporting.
- Tighten security: threat modeling, logging/alerting, backup/restore drills, access reviews.
- Make your compliance story boring: clear diagrams of data flows, module boundaries, systems of record, and who touches PHI where.
At this point your stack should look like: prebuilt plumbing + custom brains, not “someone else’s product with your logo.” Prebuilt components got you moving fast; your own codebase keeps you from getting stuck there.
Where Specode Fits in the Prebuilt-Module Landscape
By this point you’ve seen the spectrum: no-code toys, opinionated healthcare platforms, backend frameworks, and the “please don’t make me choose” mashups in between. Specode deliberately sits in a pretty narrow lane:
Healthcare-native building blocks, assembled by an AI assistant, with a real codebase you can keep, extend, or hand off to experts when things get gnarly.

Specode’s Model in One Breath
Specode is an automated platform built around reusable HIPAA-ready components: auth, portals, intake, scheduling, telehealth, EMR-lite, notifications, commerce, outcomes tracking, all designed to work together out of the box.
On top of that you get a conversational builder: you describe the clinic or program you’re trying to stand up, and it wires those building blocks into real flows instead of hallucinating random screens.
Crucially, it doesn’t trap you in config. You end up with a codebase you own — so you can keep using Specode as your spine, or take pieces and run.
How Teams Actually Use It
In practice, we see three main patterns:
- Self-serve, AI-first
Early teams use the assistant to stand up a working health app quickly: login, onboarding, provider search, intake, scheduling, video visits, messaging, basic charting, notifications. It’s a fast way to validate a model without hiring a full engineering team on day one. - Hybrid: AI + your engineers
Product and clinical folks “sketch” the app with the AI builder; engineers then refine components, layer on custom logic, and integrate external systems (EHR, labs, billing, analytics). Over time they apply the extraction playbook from earlier: keep Specode for the boring plumbing, move critical workflows into their own services when it makes sense. - Full-service for the hairy stuff
When it gets properly hard — AI agents that coordinate care, gnarly integrations with legacy EHRs, multi-system orchestration — teams bring in the Specode dev team to push beyond what the default components cover. The difference from a typical agency gig: all of that work still lands in your repo. When the engagement ends, you keep the stack, not a hostage platform.
For example, AlgoRX used this model to stand up a prescription e-commerce platform that combines eligibility screening, provider automation, pharmacy routing, and integrated payments into a single patient journey — and hit 7-figure ARR within months of launch.
You can move between these modes over time. Start scrappy with AI-driven assembly, pull in your own devs as you grow, tap the Specode team for the mission-critical or regulated pieces.
Where It Sits vs Other Options
Compared to the four patterns from earlier:
- It’s not a pure no-code builder: you’re not stuck living forever inside drag-and-drop UIs and opaque scripts.
- It’s not a closed SaaS vertical: you’re not just configuring someone else’s clinic system and hoping their roadmap matches yours.
- It borrows the good parts of backend frameworks (clean auth, PHI storage, integration patterns) but gives you a faster on-ramp via the AI builder and pre-assembled clinic flows.
If you think in 80/20 terms, Specode’s job is to give you a solid, HIPAA-ready 70–80% — and a credible path to own, extend, or completely rewrite the 20–30% that actually differentiates you, whether that’s your own engineers doing the work or ours.
If you’re currently staring at a blank stack diagram wondering how much to reuse vs rebuild, a reasonable starting point is: map your components using the maturity matrix, then see which pieces Specode can cover today and which ones you’ll want to grow into custom over time.
Frequently asked questions
Most prebuilt components cover the basics: encrypted PHI storage, audit trails, access controls, and a BAA for core services. But compliance isn’t automatic. Your team is still responsible for validating data flows, configuring permissions correctly, and ensuring any integrated systems (video, SMS, payments, analytics) are covered under BAAs as well.
Teams typically move from “nothing” to a functional MVP in weeks instead of months because core pieces like auth, portals, scheduling, telehealth, intake, and basic EMR-lite are already wired. The speed boost is real, but it still depends on how much of your workflow fits these defaults and how many integrations you need.
Yes, but only if the platform supports clean data export, code ownership, or a documented extension pathway. Without those, migration often means a partial rebuild. A good stack makes it easy to take over components as your product matures.
They help with infrastructure (auth, audit logs, PHI storage), but core FDA-facing logic usually requires custom engineering. Prebuilt workflows are rarely specific enough for regulated use cases, so most teams use them as scaffolding, not the final implementation.
You’ll see a mix of per-user pricing, per-provider pricing, per-message fees, usage-based billing for SMS/video, and paid add-ons for advanced integrations. The inexpensive MVP phase often turns into a more expensive operating cost once you grow, so it’s worth modeling a 3–5 year total cost of ownership before committing.









