White Label Telehealth Platform Guide 2026: Launch Your Branded Solution in Days
You don’t need another blog explaining why telehealth is here to stay. You already know that. But what most articles gloss over is this: custom-building a telehealth platform today makes as much sense as coding your own payment processor.
You don’t have the time—or the budget bloat—for reinvention theater. And that’s exactly where a white label telehealth platform becomes not just a convenience, but a strategic advantage.
This isn’t some “build faster with templates” fluff. It’s about launching a HIPAA-compliant, fully branded platform in 30 days, not 12 months. With Specode, you’re skipping the boilerplate and focusing on what actually moves the needle: patient experience, workflow efficiency, and bottom-line ROI.
Key Takeaways
- Why white-label is the smart shortcut: A white label telemedicine app trims 30–60% off dev time, letting you skip boilerplate and go live faster—with no tradeoffs in compliance or customization.
- How Specode accelerates time-to-value: With Specode’s modular architecture and a healthcare AI builder (build by chat → instant preview), you can launch a white-label telehealth platform that adapts to your workflows—without rewriting your tech stack.
- Who should seriously consider this route: If you’re juggling multiple care sites, scaling a mental health network, or enabling branded rollouts for partners, a telehealth white label solution gives you speed, flexibility, and full ownership of code.
White Label Telehealth Platform Overview

Market Demand for White-Label Solutions
The telehealth boom is still accelerating — and that tailwind creates a major opportunity for white-label approaches. Estimates place the global telehealth market at roughly USD 196.8 billion in 2025, with forecasts pointing to a > 5× expansion over the next decade (to more than USD 1.2 trillion by 2034) at a CAGR of ~22.5%.
Another source projects the telemedicine sector reaching USD 432.3 billion by 2032, growing at around 19% per year.
As legacy hospitals, clinics, and emerging care providers scramble to capture a slice of this growth — often under regulatory or budget pressure — the demand for fast, brandable, compliant telehealth platforms is surging. A white-label solution is how many are answering that call.
Bottom line: the market is not quiet. Telemedicine isn’t a fad. It’s a structural shift — and white-label gives providers a way to ride it without rewriting the whole software stack.
Build vs. Buy vs. White Label: Strategic Tradeoffs
For many providers, white-label strikes the “Goldilocks sweet-spot.” You avoid the development overhead and compliance complexity of a custom build, but still retain brand identity, flexibility to customize, and ability to integrate with existing systems — something off-the-shelf SaaS can’t always deliver.
As recent case studies show, white-label allows launching a fully branded, HIPAA-ready platform in under 30–45 days rather than 9–12 months.
ROI Timeline for White Label Platforms
When you strip away the buzzwords, the real question is: how fast does this thing pay for itself compared to a custom build or generic SaaS?
Recent studies and industry reports give us a few hard anchors:
- Telehealth programs in mental health have reported 315% ROI over three years, largely from reduced crisis escalations and better adherence.
- Remote patient monitoring and virtual programs routinely see 4–7× ROI, sometimes breaking even in under 2 months once patient panels hit scale.
- Across providers, telehealth adoption has driven an average 23% revenue increase and 31% reduction in operational expenses, with a mean payback of ~6.8 months.
By contrast, building your own telemedicine stack from scratch typically takes 4–8 months of development plus integration and rollout, and many organizations report ~23 months from “we need telehealth” to full-scale deployment.
That’s a 2-year runway before you’re really compounding returns.
A white-label telehealth platform compresses that timeline roughly as follows:
Month 0–1 – Configuration, Not Construction
- Map your workflows onto a pre-built, HIPAA-ready core (video, scheduling, messaging, auth).
- Brand the patient and provider portals, configure roles, and plug in billing/EHR where needed.
- You’re spending a fraction of custom dev cost, because you’re not paying to reinvent commodity features.
Month 1–3 – Revenue Starts Landing
- First cohorts of patients and providers onboard; visit volume stabilizes.
- On a per-visit basis, telehealth episodes are typically ~$100 cheaper than in-person for payers and employers, and can be $80–$120 cheaper vs. traditional acute care in some programs.
- A meaningful share of follow-ups, chronic care, and triage shifts online, so you’re capturing both new revenue and freed-up physical capacity.
Month 3–6 – Operational Efficiency Compounds
- No-show rates drop, staff time per visit shrinks, and overhead (room turnover, front-desk load, overtime) comes down.
- This is typically where practices in surveys hit cashflow break-even on their platform investment, lining up with the ~6–9-month payback windows reported for telehealth and white-label scheduling/visit solutions.
Month 6–12 – Beyond Payback: Margin and Scale
- Telehealth stabilizes at 10–20%+ of visit volume (many systems sit in the 13–17% range long-term), which becomes a durable, higher-margin slice of your service mix.
- At this point, the original platform cost is usually fully recovered; additional optimization (better triage, bundles, memberships) drives incremental margin rather than just “covering the tool.”
The spreadsheet version: custom builds often start to prove ROI around the time a well-implemented white-label deployment has already paid itself back and moved on to “how do we use this channel to spin up the next service line?”
If you’d like, next step we can align this section more explicitly with how Specode cuts that Month 0–3 window (e.g., “build-by-chat → instant preview”) without turning it into a sales pitch.
Success Metrics and KPIs
If you launch a white-label telehealth platform today, here are the KPIs you should track to measure success and justify the investment:
- Time to launch — the faster you go live, the sooner you start capturing value (weeks vs months).
- Adoption rate — how many existing patients (or new users) switch to the platform; high adoption suggests convenience & usability.
- Visit / session volume — frequency of telehealth visits per patient or provider.
- No-show / cancellation rate — telehealth should reduce friction; lower no-shows means higher utilization.
- Cost per consult — reductions vs in-person visits (staff time, admin overhead, overhead rental/space savings).
- Customer acquisition cost (CAC) / Lifetime value (LTV) — with branding and flexibility, you can optimize for retention, upsells (e.g. subscriptions, packages), or ancillary services.
- Operational efficiency — measured through admin time saved, fewer manual workflows, secure compliance maintenance, faster billing cycles.
- Scalability / infrastructure cost per user — as you add users, how much does marginal cost grow? White-label modular platforms often yield lower marginal cost thanks to reuse and built-in interoperability.
Understanding White Label Telehealth Solutions
Building a telehealth app from scratch used to be the gold standard—until teams realized they were burning six figures and 9+ months on the boring parts: auth, video, messaging, appointment workflows, and all the HIPAA plumbing nobody actually markets.

A white label telemedicine platform changes the model. Instead of building from the ground up, you start from a proven core: patient and provider portals, virtual visits, scheduling, payments, messaging, analytics—all wired for compliance—then shape it around your brand and workflows.
For health systems and digital health companies who need a branded digital health solution this year, not “after the next budget cycle,” that’s a very different game.
White Label vs. Custom Development Deep Dive
Custom development gives you total control—but at a very real cost. When you’re building from the ground up, you’re not just paying for features; you’re paying for requirements discovery, architecture, compliance hardening, integrations, and years of ongoing maintenance. The first release is usually the most expensive prototype you’ll ever ship.
A white label approach starts from an opinionated, battle-tested baseline:
- Core telehealth flows (intake → triage → visit → documentation → billing) are already implemented.
- Security, HIPAA safeguards, and auditability are baked into the platform instead of bolted on at the end.
- Your team spends its energy on differentiation—clinical model, care programs, UX—rather than reinventing generic infrastructure.
You still get room for edge cases and custom integrations, but you’re not waiting 12–18 months to see if the fundamentals even work.
White Label vs. SaaS Platform Comparison
Off-the-shelf tools promise speed: “sign up today, launch tomorrow.” That’s fine if you’re a small clinic willing to live with someone else’s brand, workflows, and roadmap. It’s less fine when you’re a health system trying to run serious digital health initiatives under your own flag.
Generic SaaS platforms typically come with:
- Fixed branding and UX that can’t reflect your care model.
- Limited integration paths (or expensive “enterprise” tiers) to talk to your EMR, CRM, or rev-cycle stack.
- Roadmap risk: your core digital health solutions now depend on a vendor’s priorities.
A white label telehealth platform sits between pure SaaS and pure custom:
- You get an owned, branded experience across web and mobile.
- You can configure flows, roles, and data models to match your service lines.
- You can still move quickly because 80% of the baseline telehealth logic is already wired up.
In other words: you’re not trapped in someone else’s product, but you’re also not paying to build your own from zero.
Private Label vs. White Label Distinctions
“White label” and “private label” often get used interchangeably, but there’s a useful distinction:
- White label usually means a shared core product that multiple organizations can brand and configure, with a common underlying codebase and infrastructure.
- Private label implies more isolation—sometimes a dedicated environment, deeper customization, or stricter data and integration boundaries tailored to a single organization or network.
For most health systems and care networks, the interesting question is not the label but the control surface:
- Can you enforce your own security and governance policies?
- Can you model your specific roles and care pathways?
- Can you scale to multiple service lines or regions without creating a Frankenstein stack?
Good white label platforms give you enough “private label” control where it actually matters—data, roles, integrations—without losing the economies of reuse.
Technology Stack Considerations
Under the hood, a serious white label telemedicine platform is more than a video widget and a calendar. The stack typically spans:
- Frontend applications for patients, providers, and admins (web + mobile), built for accessibility and clinical-grade reliability.
- Backend services for identity, permissions, scheduling, visits, messaging, and payments.
- Data and compliance layer with PHI-aware schemas, audit logging, retention policies, and encryption in transit and at rest.
- Integration fabric for EMR/EHR systems, billing, eRx, lab vendors, and analytics.
- Extensibility points so you can plug in things like AI intake, decision support, or remote monitoring without rewriting the core.
This is where platforms start to diverge. Some are glorified video chat with a logo slapped on. Others are closer to a healthcare-grade app framework designed for long-term reuse across multiple programs. When you’re evaluating options, you’re not just buying features—you’re buying an architecture your team has to live with for years.
Total Cost of Ownership Analysis
Upfront license fees are the visible part of the iceberg. Total cost of ownership is everything else:
- Months of engineering time spent on infrastructure, not care models.
- Compliance reviews, security remediation, and penetration testing.
- Integration work with EMR, billing, CRM, and reporting systems.
- Ongoing maintenance as regulations, payer rules, and clinical workflows evolve.
With a white label approach, a large chunk of that cost moves from “custom project” to “platform capability”: you amortize security, compliance, and core feature development across many deployments instead of paying for it alone.
That’s why, over a 3–5-year horizon, white label often beats both raw custom builds and loosely stitched-off-the-shelf tools on TCO—especially when your telehealth stack is supporting multiple service lines and regions.
If you need to go even deeper into budgets and resourcing trade-offs, our telemedicine app development guide breaks down the cost structure of building a telehealth app from scratch vs leveraging a more opinionated foundation.
Looking to launch a compliant telehealth solution under your brand? Let’s build it together.
Comprehensive Feature Architecture for White Label Telehealth
The beauty of using Specode’s white label telehealth platform is that you’re not stuck with a static product. Every core feature listed below is part of a modular system—continuously updated, HIPAA-compliant, and customizable to fit your clinical workflows today and whatever your roadmap throws at you tomorrow.

Frontend Architecture and Customization
This is what your users notice first — and judge you for the fastest.
- Fully brandable patient and provider portals (colors, typography, logo, navigation)
- UX variations for specialty use cases (e.g., behavioral health, urgent care, home health)
- Role-aware UI components with clinical task prioritization
- Mobile-first layouts with accessibility built-in (WCAG 2.1 AA)
Because when digital health solutions feel generic, users assume care will feel generic, too.
Backend Infrastructure Components
White label ≠ “front-end lipstick.” Behind the UI, you get a real healthcare-grade engine:
- Microservices for scheduling, encounters, documentation, and messaging
- PHI-aware data model aligned to clinical workflows
- Unified identity and permissions service (SSO, MFA, OAuth, SAML support)
- Task orchestration for follow-ups, escalations, and longitudinal care
This is what converts a telehealth app from a widget into a clinical system.
Essential Components (Clinical Frontline Features)
Any serious private label telemedicine solution needs to nail the basics—because “we’ll fix it post-launch” isn’t a strategy, it’s a budget leak. Here’s what your MVP actually needs:
- Secure video consultations: Encrypted, compliant, and resilient on low bandwidth. No awkward pixelated freeze-frames during urgent care.
- Asynchronous chat and real-time messaging: For pre-visit intake, post-visit follow-up, or mid-visit clarifications.
- EMR-lite or full EHR integration: View, edit, and sync patient data seamlessly—yes, including SOAP notes and labs.
- Scheduling and reminders: Custom time slots, availability rules, and push/email notifications to keep no-shows low.
- Branded patient portal: Give users access to their health data, care plans, messages, and appointments. And yes, it should work beautifully on a mobile app.
This foundation powers most of the top 18 telehealth apps for doctors and patients—and with Specode’s white label telehealth platform, you get it pre-built, pre-secured, and fully brandable.
Infrastructure and Administrative Controls
Let’s talk about infrastructure—the stuff your compliance officer will grill you about.
- Role-based access controls: Segment permissions for front-desk, clinicians, billing, and admin staff.
- Admin dashboards: See platform usage, billing data, and user analytics in real time.
- Secure payments: PCI-compliant, with co-pay capture and payment histories.
- Rich provider and patient profiles: Upload credentials, NPI, insurance info, and medical history.
No Frankenstack. No duct-taped plug-ins. Just cohesive modules that actually play nice together.
Security and Compliance Features
Compliance isn’t a checkbox — it’s failure prevention.
- HIPAA-aligned data retention and access logging
- Encrypted communication (TLS 1.2+ end-to-end)
- BAA support + automated audit evidence
- Least-privilege defaults with breach containment patterns
- Zero trust network posture, segmentation, and key rotation
The part that keeps your name out of news headlines.
Bonus Capabilities (Care Expansion Modules)
This is where a private label telemedicine app goes from functional to future-ready:
- ePharma integration: Prescribe meds digitally with formulary checks baked in.
- Remote patient monitoring: Connect to devices (BP cuffs, glucometers, wearables) and track vitals.
- Labs ordering and results delivery: Trigger lab orders and deliver results in the patient portal.
- Virtual waiting room: Triage patients before they enter a virtual consultation, boosting provider efficiency.
Integration Architecture
A modern telehealth platform must work inside the ecosystem, not outside it:
- FHIR / HL7 bi-directional EHR sync
- Billing + clearinghouse compatibility
- Pharmacy / lab integration
- Real-time eligibility and claims insight
- Third-party API governance and monitoring
See alignment with your healthcare mobile app development guide — no hidden integration debt.
Scalability and Performance Features
Because success should never cause downtime.
- Auto-scaling infrastructure across regions
- Database sharding for multi-site health systems
- Queueing and retries for peak clinical hours
- Uptime SLAs with continuous deploy safety rails
From 5 providers → 5,000 without needing a platform rewrite.
Mobile vs. Web Platform Capabilities
In telehealth, location is a variable, not a constraint.
Web 🖥 — hospital workstations, long-form charting
Mobile 📱 — in-home care, urgent consults, messaging touchpoints
Shared:
- Unified codebase = parity in features
- Secure offline access modes
- Device-aware UI for wearables + sensors
Care happens everywhere — your platform should too.
Modular Build = No Feature Bloat, Just What You Need
With Specode, you get plug-and-play components tailored to your workflow. Skip what you don’t need, extend what you do, and scale as you grow. No monoliths, no regrets.
Need specific features in your telemedicine app? Our experts will tailor them to your practice.
Building the Business Case for White Label Telehealth
Telehealth is no longer a side project; it’s a core service line. The global telehealth market is estimated at ~$123B in 2024, projected to reach $455B by 2030 at ~24.7% CAGR.
Telehealth already accounts for up to 17% of outpatient/office visits in the U.S. and has held that share since 2020. In that context, the question isn’t whether to invest, but how to do it without blowing up capex and timelines.

Financial Analysis and ROI Projections
Telehealth can generate serious returns when it’s wired into real care programs instead of living as a one-off pilot:
- Mental health services using telehealth report 315% ROI over three years, with big drops in crisis events and better adherence.
- Remote patient monitoring programs typically see 3–5× ROI with 2–3-month break-even at modest panel sizes.
A white label telehealth stack doesn’t magically create those numbers, but it dramatically lowers the cost and time to plug into the same reimbursement codes and care pathways that drive that ROI (RPM, CCM, tele-psych, hybrid primary care).
Time-to-Market Advantages
This is where white label quietly destroys custom builds:
- Custom telemedicine apps often take 4–12 months to reach production.
- Some dev shops estimate ≥120 days minimum even for a lean custom telehealth MVP.
- By contrast, white label telemedicine solutions routinely launch in 1–3 months, with some suites going live in ~2 months depending on customization.
In a market where telehealth is already a stable share of visits, being 6–9 months late means handing those encounters—and that recurring revenue—to competitors.
Risk Mitigation Strategies
A credible business case also has to answer: what could go wrong, and how do we contain it? White label helps on three fronts:
- Delivery risk – You’re starting from a proven codebase and integration patterns instead of betting on a greenfield build.
- Compliance risk – HIPAA-grade logging, encryption, and workflows are inherited from the platform instead of reinvented (and audited) from scratch.
- Execution risk – You can pilot in one specialty or region, then expand, instead of committing a full capex roll-out up front.
The result is less “big bang go-live,” more controlled rollout with measurable checkpoints.
Competitive Advantage Assessment
Telehealth is growing quickly, but not evenly. Enterprise systems, retail clinics, and digital-first players are all chasing the same patients in a market compounding at ~25% annually.
A white label approach gives you:
- Brand control – your own front door, not a vendor’s portal.
- Service-line agility – spin up behavioral health, chronic care, or employer programs on the same core.
- Data leverage – unified telemetry across virtual and in-person care instead of siloed vendor dashboards.
That’s the difference between “we also offer telehealth” and “virtual is a core distribution channel.”
Funding and Investment Considerations
Digital health is still getting funded: $10.1B in venture dollars in 2024 across 497 deals, with investors skewing toward earlier-stage, capital-efficient plays. Meanwhile, 42% of 2024 digital health funding flowed into AI-focused companies layered on top of existing infrastructure.
Put bluntly, investors are tired of bloated, multi-year platform builds. A white label telehealth strategy with:
- clear capex bounds,
- 3–12-month ROI modeled off existing telehealth/RPM benchmarks, and
- a roadmap for layering AI and programmatic care on top
is far easier to underwrite than “we’ll spend 18 months building our own stack and see where we land.”
White Label Telehealth Implementation Roadmap
Going live with a white label telehealth platform shouldn’t feel like reconstructing a hospital from scratch. The goal is simple: launch fast, launch safely, scale without regrets. This roadmap keeps velocity high while keeping compliance and workflow integrity intact.
Discovery and Requirements Phase
This isn’t a feature wishlist. It’s ops meets care delivery.
- Identify clinical programs (e.g., urgent care, mental health, CCM, RPM)
- Map patient + provider journeys (actual workflows → not hypothetical happy paths)
- Define roles + permission scopes (front desk, MA, NP/MD, billing, admin)
- Confirm regulatory posture (multi-region waivers, PCMH rules, credentialing flows)
Outcome: a deployment-ready scope tied to real reimbursements and usage volumes.
Customization Planning
Where you shape the product around your differentiation, not commodity features.
- Component selection: what’s in MVP vs. deferred to Phase 2
- UX tailoring: specialty-specific triage, templates, documentation
- Analytics and reporting hooks to measure success before launch
- Multi-brand or enterprise network planning (if scaling across affiliates)
The mantra here: start with what makes you money, refine what makes you unique.
Branding and Design Process
Patients don’t use your tech — they judge it.
- Brand styling applied to all surfaces: apps, portals, onboarding, notifications
- Accessibility-first refinements (font scale, contrast, cognitive load adjustments)
- Mobile design review: most encounters start on a phone, not a workstation
Visual trust is clinical trust — particularly in behavioral health and chronic care.
Integration Strategy Development
Telehealth isn’t a silo. It needs to fit into the financial + clinical plumbing you already have.
- EHR and billing connections defined in detail (directionality, conflict resolution)
- Labs and pharmacy connectivity (if relevant in Day 1 flows)
- Insurance eligibility and claims data mapped early, not post-launch
- API governance: versioning, failures, uptime monitoring
This prevents the classic: “Revenue isn’t posting correctly — who owns this mess?”
Testing and Quality Assurance
Test the care model, not just the UI.
- End-to-end simulations: intake → triage → visit → documentation → billing
- Negative path testing: no-shows, disconnects, insurance denial paths
- Security validation: RBAC correctness, audit trails, access revocation
- Load checks for Monday morning surges and seasonal peaks
Every bug caught in QA saves 10× effort after clinicians are in production.
Launch and Deployment Strategies
Release plans designed for minimum risk, maximum confidence.
- Soft launch: one region/specialty → collect utilization + retention signals
- Provider onboarding playbook (training takes minutes, not hours)
- 24–72 hour hypercare post-launch for rapid-fire fixes
- Phased feature unlocks based on measured readiness
Success = predictable go-live + measurable value in the first quarter.
The Specode Advantage: AI-Powered White Label Development
Specode isn’t just another white label telemedicine platform. It’s an automated platform with reusable HIPAA-compliant components and a conversational AI assistant, designed to help health-tech teams assemble production-grade apps faster — without vendor lock-in and at a fraction of traditional telemedicine app development cost.

Component Library Overview
Instead of reinventing healthcare plumbing, you assemble using a constantly expanding library of pre-built, HIPAA-aware modules — patient dashboard, intake, scheduling, secure messaging, video visits, payments, outcomes tracking, pharmacy flows, and more.
What it means for you:
- Less backend repetition → faster delivery
- Every component already designed for PHI workflows
- Swappable modules to support evolving care models
- Code ownership from day one — no platform ceiling
The library grows continually as we ship new components to help healthcare professionals bootstrap and scale telehealth use cases.
Pre-Built, Pre-Tested, HIPAA-Compliant Components
Every component is:
- Field-tested across real clinical deployments
- Built with PHI-safe defaults (audit trails, encryption, access controls)
- Designed for provider workflows, not generic SaaS edge cases
You get enterprise-grade infrastructure without enterprise delays — assemble from excellence instead of building from scratch.
AI Builder Technology Explained
Specode’s platform AI:
- Builds workflows through natural-language dialogue
- Acts as a developer + system architect, advising on best paths
- Wires components, data models, validation, notes, and UI in seconds
- Uses guardrails based on 10+ years of HIPAA-grade app development
- Leverages industry-benchmark AI for code generation and “vibe-correct” UX
The results: Prompt → preview → tweak → production-ready app. No AI magic — sequence and ruthless focus.
Also: AI agents in healthcare can be deployed inside the product (triage, documentation assistance, eligibility checks), not just in the build process.
Customization Framework
When your workflows get complex — good.
- Full control over components (fields, logic, data, UI, roles)
- Custom code where needed — your team or ours
- Deep system integrations (EHRs, labs, pharmacies, RPM devices)
- Full branding (logo, themes, layout, typography)
White label telemedicine platform doesn’t mean “one look fits all” — it means your front door, your operations, your care model.
Security Architecture
Security is not optional in healthcare — it’s existential.
- HIPAA-aligned logs, retention, permissions built-in from day one
- End-to-end encryption + PHI-restricted data paths
- Role-based access controls enforced centrally
- Only HIPAA-compliant vendors involved in telehealth, payments, and data exchange
- BAA support and breach-prevention patterns
Compliance is the default, not a late-game scramble.
Development Workflow
Faster cycles, lower telemedicine app development cost, no compromises:
1️⃣ Build by talking to the AI
2️⃣ Preview UX live within minutes
3️⃣ Iterate on flows, rules, and structure
4️⃣ Connect your own data early to see real PHI behavior
5️⃣ Specode team steps in when you’re ready for live deployments (PHI, EHR connections)
6️⃣ Production launch with code ownership and full compliance review
You stay in control. We remove friction.
Support and Maintenance Model
You’re not left alone once you launch:
- Email + asynchronous support at all tier levels
- Product lead guidance for complex feature planning
- Full-service enhancements + maintenance at higher tiers
- Continuous delivery of improvements as the platform evolves
Ongoing subscription = ongoing upgrades — zero legacy drag.
10× Faster App Launch with AI-Assisted Assembly
Traditional dev moves like a fax machine in a 5G world.
With Specode:
- Up to 10× faster vs. hand-coded stacks (internal benchmarks)
- 30–60% shorter cycles → direct savings on engineering costs
- Near-instant pivots without re-architecting
- Go from requirements → pilot-ready in weeks, not quarters
That speed shows up on the P&L — earlier revenue, fewer sunk costs.
Real-World Example: DyadSync & AlgoRX
DyadSync used Specode to turn chaotic, spreadsheet-and-text–based anesthesiologist scheduling into a focused web platform for freelance surgeons and anesthesiologists. Role-based onboarding, smart scheduling dashboards, contextual in-app messaging,
Stripe-powered payouts, feedback flows, and admin analytics were all assembled from Specode components—so they could streamline case coverage and boost income visibility without funding a multi-quarter custom build.
AlgoRX built a Shopify-style medication storefront on top of our telehealth white label framework. Patients move through guided onboarding and eligibility screening, add multiple medications to a single cart, and check out via PCI-compliant NMI payments, while providers handle credentialing, automated reviews, and secure chat from one dashboard.
The result: a lean, scalable ePharma platform for non-controlled medications that reached $1M+ in sales by month 2, hit 7-figure ARR by month 3, and delivered a 12× ROI using Specode’s components.
These aren’t MVPs duct-taped together. They’re branded, production-grade deployments that show what a white label telehealth solution can do when you start from healthcare-native components instead of a generic app skeleton.
Launch your white label telehealth solution in record time — let’s talk timelines.
White Label Solutions by Healthcare Vertical
From enterprise health systems to nimble digital-first providers, white label telemedicine software creates a faster path to market—with fewer dev headaches and far more control over the patient experience. In other words: who is white label telemedicine platform for in practice?

Enterprise Health Systems
Large hospitals and IDNs need more than a pretty app; they need brand control, EHR integration, and HIPAA discipline at scale. With Specode, enterprise teams roll out custom-branded virtual care across service lines without building yet another monolith.
- Branded patient + provider portals on top of existing Epic/Cerner/other EHR flows
- Plug-and-play scheduling, EMR-lite, secure messaging, and telehealth
- Multi-site configuration for affiliates and partner clinics
Use case: A regional hospital chain extending branded telehealth to dozens of satellite clinics without duct-taping third-party platforms together.
Specialty Practice Networks
Multi-location groups in cardiology, oncology, urgent care, pain, women’s health, etc. need workflows tuned to their specialty, not generic templates.
Specode lets them launch virtual pathways for triage, follow-ups, chronic care, and procedures on a shared backbone—so each practice gets its own flavor while operations stay manageable.
Use case: A multi-state specialty network standardizing intake, consults, and follow-ups while allowing each clinic to localize content and availability.
Behavioral Health Platforms
Mental health and addiction care live or die on trust, privacy, and continuity. Specode’s modular stack supports:
- One-on-one and group therapy flows
- Longitudinal tracking (mood, goals, meds)
- Hybrid models (tele-psych + in-person)
Use case: A multi-state group practice delivering mental health services across time zones, with role-based access, flexible scheduling, and secure messaging baked in.
Direct-to-Consumer Healthcare
DTC brands need consumer-grade UX + medical-grade compliance—fast.
White label telemedicine software on Specode gives DTC players subscription programs, asynchronous consults, labs and ePharma flows, and follow-up automation without building their own stack from zero.
Use case: A virtual clinic offering cash-pay chronic care bundles with app-based onboarding, telehealth, and medication management.
B2B Healthcare Technology Companies
If you’re a healthcare app development services company, PBM, TPA, or employer-benefits vendor, speed and reuse matter more than hero engineering.
Specode lets B2B players ship client-branded platforms in weeks, not quarters, while reusing the same hardened infrastructure across accounts.
Use case: A services firm delivering white label telemedicine platforms to payers and employer plans, customizing only the 20% that’s client-specific.
International Healthcare Markets
Cross-border telehealth must respect local regulations, languages, and payer models.
Specode supports multi-region deployments with localization, configurable consent flows, and region-aware logic—so you can reuse core components while adapting to country-level rules.
Use case: A virtual-first provider rolling out in the U.S., UK, and EU with shared components but country-specific onboarding, pricing, and compliance.
Bottom line: off-the-shelf SaaS can’t flex this broadly. A modular, Specode-powered white label telemedicine platform gives each vertical what it actually needs—without forcing everyone into the same cookie-cutter app.
Whether you’re a provider or a partner — we’ll help you deliver high-quality virtual care.
Enterprise Integration and Customization Framework
Most white label platforms offer surface-level branding and call it innovation. But real digital health solutions have to plug into serious infrastructure — clinical records, billing rails, pharmacy networks, lab vendors, and care-coordination systems — without forcing a rewrite of your entire stack.

Specode was built for that world.
Web, mobile, satellite deployments, multi-brand configurations — our backend stays composable, not rigid. This isn’t lipstick on a patient portal; it’s a technical foundation for health systems that can’t afford brittle integrations or vendor lock-in.
EHR / EMR Integration Strategies
Your clinical system remains the source of truth. Specode’s approach: meet your EHR where it lives — not the other way around.
- FHIR and HL7-based interoperability
- Secure API pipelines with audit-grade data lineage
- Patient context hand-offs between telehealth encounters and in-person workflows
- Direct mapping to care pathways (triage → documentation → coding → billing)
Whether you think in Epic App Studio or Cerner Ignite, we prevent fragmentation and duplication of clinical data — a universal pain point in building a telehealth app from scratch.
Payment Gateway Integration
If you can’t get paid, you can’t scale. Specode makes financial plumbing invisible:
- PCI-compliant payment processing
- Real-time eligibility & copay estimates
- Support for subscription and per-visit billing
- Revenue tracking that folds neatly into your RCM analytics
No “call your vendor to enable it next quarter” surprises.
Laboratory System Connections
Telehealth doesn’t stop at Zoom calls. Diagnostics matter.
- Orders and results exchange
- LOINC-driven mapping for labs and vitals
- Notification hooks to trigger provider follow-up
- Multi-state lab partner support
This is where many off-the-shelf tools collapse — workflows get stuck at the “lab slip” stage.
Pharmacy Network Integration
Virtual care without prescriptions = urgent care with no door.
Specode supports:
- eRx workflows aligned with regional rules
- Medication history retrieval
- Dynamic formulary controls
- Specialty pharmacy routing
This isn’t just “send a script” — it’s clinical decision continuity.
Insurance Verification Systems
Coverage ambiguity kills appointment conversion.
We automate the boring parts:
- Eligibility checks via clearinghouses
- Claims lifecycle visibility
- Denial triggers → tasking and remediation
- Payer-specific metadata for compliance
This directly improves margins — CFO-approved ROI territory.
Third-Party API Management
When your care model evolves, your platform should too.
- Plug-in AI modules for triage or documentation
- Remote monitoring devices sync via secure API mediation
- Role-aware integration governance to prevent accidental PHI leakage
- Centralized monitoring for vendor uptime + security posture
This keeps your architecture consistent with your healthcare mobile app development guide — instead of a pile of duct-taped SaaS.
Specode doesn’t ask your infrastructure to do yoga. Our white label approach adapts to how your organization already delivers care — and how you plan to deliver it next year.
Want a scalable backend that bends — not breaks?
Compliance and Security in White Label Platforms
In healthcare, integration isn’t the hard part — compliance and operational resilience are. A credible white-label approach must deliver the same governance, auditability, and patient-safety guarantees as in-house clinical systems. That means architecture and process, not marketing claims.

HIPAA Compliance Architecture
True HIPAA support isn’t a badge — it’s a design system:
- Isolation of PHI using role-scoped access controls and tenant-aware data segmentation
- Immutable audit trails for every create/read/update action tied to user identity
- Data minimization enforcement so only clinically necessary information flows into each component
- Secure identity planes separating authentication from care delivery (SSO/OAuth/SAML support)
- Automatic least-privilege defaults to contain blast radius of account compromise
The goal: no feature is allowed to exist outside HIPAA-aligned guardrails.
International Healthcare Regulations
White-label platforms succeed when they localize compliance to jurisdiction without losing architectural consistency:
- GDPR-driven consent models and data residency enforcement
- Region-specific retention windows (EU vs US vs APAC)
- Granular controls for cross-border clinical information exchange
- Support for country-specific certification layers (e.g., UK DSPT, Canadian provincial rules)
A compliant platform should abstract regulatory differences — not ask product teams to rewrite code for each market.
Data Privacy and Protection
Privacy is the assurance that data access aligns with intent — not convenience:
- End-to-end encryption across transit/intra-service links
- Segregated keys + automatic rotation schedules
- Event-driven anomaly detection on data patterns (e.g., mass exports, out-of-hours access)
- Formal governance of third-party access with revocable credentials and scoped tokens
Modern telehealth isn’t just about encryption — it’s about preventing privilege creep and enforcing contextual access.
Security Audit and Monitoring
If you can’t observe the system, you can’t defend it:
- Continuous vulnerability scanning and dependency inspection
- SIEM pipelines with alerting on identity anomalies and failed access bursts
- Structured log formats for compliant external audit (SOC 2 alignment)
- Regular penetration tests with remediation SLAs
Compliance is never “granted” — it’s continuously proven through telemetry.
Disaster Recovery Planning
Healthcare downtime isn’t an inconvenience — it’s a clinical risk. A serious white label telemedicine platform needs:
- Multi-zone failover capabilities
- Automated backup + tested restore procedures
- RTO/RPO targets meaningful for patient safety (minutes, not hours)
- Graceful degradation options for telehealth workflows (e.g., alternate comms channels)
Operational resiliency must be designed and rehearsed, not aspirational.
Compliance Documentation
If it isn’t documented, it doesn’t exist — at least not to risk officers:
- Real-time compliance status dashboards for PHI workflows
- Traceable lineage of controls from requirements → implementation → monitoring
- Pre-written policy templates aligned to HIPAA/GDPR operational standards
- Evidence bundles available for vendor assessments and payer credentialing
This reduces weeks of paperwork into hours of structured validation — a competitive edge when selling enterprise healthcare.
White Label Telehealth Platform Pricing Guide
This section unpacks the real economics behind white-label telehealth platforms — not as a marketing brochure, but as a decision-maker’s financial framework. We walk through models, costs, hidden risks, and ROI levers in a way that helps you build a credible business case (or project pitch).
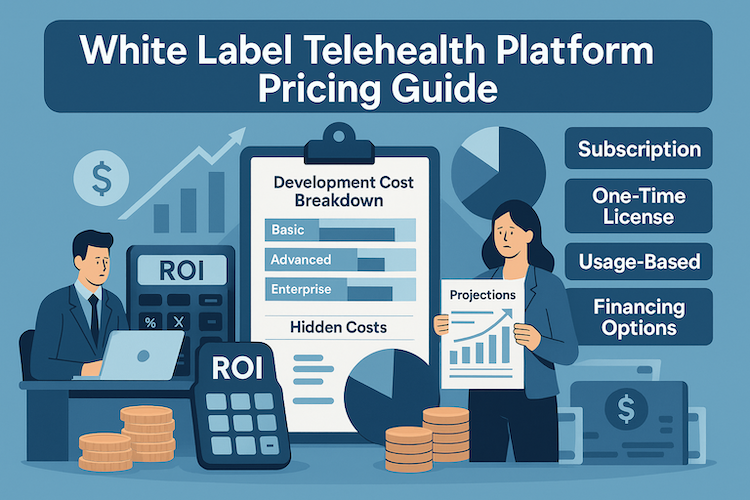
Pricing Models Comparison
White-label telehealth platforms generally adopt one of several pricing models — and the right choice depends on your scale, risk tolerance, and growth plans.
- Subscription / SaaS-style model — you pay a regular license fee (monthly or annual) per user or per facility. Simple, predictable, but often limits customization or feature ownership.
- License + customization fee — base license covers core modules; additional sums cover custom integrations, branding, or tailored workflow logic.
- Usage-based / volume model — costs scale with patient volume, sessions, or data throughput; ideal for pay-per-visit telehealth or usage-heavy models without upfront burden.
- Upfront license + maintenance/hosting contract — trade initial capital expense for long-term control and flat operational cost; attractive for enterprise health systems or large specialty networks.
Each model carries trade-offs: subscription models minimize upfront risk but may limit flexibility; license-based models maximize control but shift risk/cost up front. White-label providers that deliver code ownership (like Specode) often favor the latter — giving operators both long-term flexibility and predictable TCO (total cost of ownership) when planned right.
Development Cost Breakdown
The cost to build telemedicine software from scratch (which you avoid with white-label) remains surprisingly variable. Estimates for custom telehealth apps in 2025 span from ~$40,000 for a basic MVP to $300,000+ for a full-featured, enterprise-grade system.
Breaking down costs:
With a white-label telemedicine platform, much of that cost becomes license or onboarding — not full custom engineering. That dramatically reduces your telemedicine app development cost while preserving enterprise-grade capability.
With Specode, most teams can get started for as little as $250 per month, turning what used to be a six-figure build into a predictable operating expense.
Operational Cost Analysis
Once live, a telehealth platform carries recurring operational expenses. Typical costs include:
- Hosting and cloud infrastructure (storage, video bandwidth, backups)
- Security, compliance upkeep (audits, encryption, backups)
- Support, maintenance, updates, bug fixes
- Third-party API usage (video, payments, SMS, analytics)
- Regulatory support (state/province compliance changes, data residency if cross-border)
For example, research shows that annual operating costs for telehealth services often fall between ~US$137,000 and $1.2 million — depending on scale, services offered, and user volume.
Additionally, vendors often recommend budgeting 15–20% of initial development cost annually for maintenance and compliance upkeep.
The bottom line: ongoing costs can outpace upfront development over time — but with a white-label, modular stack, much of the overhead stays predictable and contained.
Hidden Cost Considerations
Even with a white-label platform, some costs tend to be overlooked or underestimated — often where projects derail:
- Compliance scope creep — additional costs for integrations, PHI handling, multi-jurisdiction data policies, user training, audits.
- Integration entropy — as you add EHRs, labs, pharmacies, APIs; maintenance and error handling cost more over time than initial build.
- Scalability overrun — user growth or data volume spikes can blow up infrastructure cost or require re-architecture.
- Support and change management — onboarding providers, training staff, documentation, help desk, version upgrades.
- Regulatory drift — evolving healthcare regulations (privacy, data residency, telehealth reimbursement rules) require ongoing compliance investment.
Ignoring these can make even a “cheap” build end up expensive — which is why transparency in total cost of ownership (TCO) matters more than low upfront quotes.
ROI Calculator and Projections
Here’s an example of how ROI can look over 12–24 months with a white-label platform vs custom build:
- Upfront cost (custom): $200k — white-label: $40–60k (license + minimal onboarding)
- Monthly ops/maintenance: $10–20k (cloud + compliance + staff)
- Revenue per consult: assume $75 average, 5000 consults/year → $375k revenue
Even conservatively, a white-label deployment can break even within 6–12 months, while a custom build might take 18–24 months — and still carry higher tech debt, maintenance overhead, and scalability risk.
Because white-label reduces both capex and time-to-market, ROI is front-loaded — which matters if you’re pitching to executives, investors, or payers with limited runway.
Financing Options
You don’t always need to foot the entire bill upfront. Common approaches include:
- License-plus-subscription: low upfront onboarding cost, predictable recurring fees, avoids major capex.
- Revenue-share or per-visit pricing: you pay based on usage — ideal if you expect slow ramp or want to align costs with growth.
- Staged rollout funding: allocate budget per phase — MVP, pilot, expansion — to limit risk and spread out investment.
- Mixed build + white-label hybrid: use white-label for core workflows, build customized modules over time — hybrid financing smooths cash flow.
These options make telehealth deployment accessible for small practices, growing networks, or enterprises testing a new line of business — without needing massive balance sheet commitment upfront.
Bottom Line: White-label telehealth platforms often deliver the sweet spot between cost control, speed, compliance, and scalability. If you map out license vs ops vs revenue carefully — and plan for hidden costs — you’re looking at a lower-risk, faster-payback path to launching digital health solutions at scale.
Technical Architecture of Modern White Label Platforms
Under the hood, a serious white label telehealth platform should look a lot closer to a modern banking stack than a glorified Zoom wrapper. Here’s what “grown-up” architecture actually means in this space.
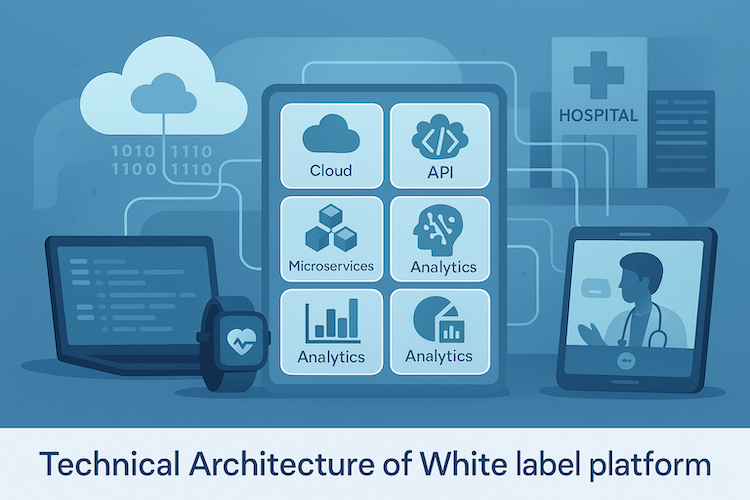
Cloud Infrastructure Options
Most production telehealth deployments land on a major cloud (AWS, GCP, Azure), but the real decision is about isolation and control:
- Single-tenant per customer: higher isolation, simpler compliance story, more predictable performance.
- Logically multi-tenant: shared infra with strict tenant boundaries; cheaper but requires mature security engineering.
- Hybrid: shared app layer, isolated data and PHI services per tenant or region.
For health systems with strong infosec teams, the critical questions aren’t “which cloud?” but:
- Where does PHI actually live?
- How is data residency enforced by region?
- Can we move to our own cloud subscription later without rewriting the app?
If a platform can’t answer those clearly, it’s not “enterprise” no matter what the sales deck says.
Microservices vs. Monolithic Architecture
Pure monoliths die the minute you add your third integration; pure microservices drown smaller teams in operational overhead. The sweet spot for telehealth is modular monolith → selectively split services:
- Keep core domain flows together (auth + roles, scheduling, encounters, messaging).
- Split out high-churn or high-risk domains: payments, notifications, video, integration brokers.
- Standardize cross-cutting concerns (logging, auth, tracing) so every service doesn’t re-solve security.
If your white label vendor can’t explain which boundaries they’ve actually drawn — and why — you’re buying future tech debt.
API-First Development Approach
For a white label telemedicine platform, “API-first” is not a buzzword, it’s survival:
- All core capabilities (intake, visits, messaging, billing, outcomes) exposed via versioned APIs.
- Clear resource contracts for patients, providers, encounters, orders, payments.
- Web + mobile + internal tools talk to the same API surface, so behavior is consistent.
This is what lets you:
- Attach your own portals or mobile apps later.
- Wire the platform into EHRs, CRMs, ERPs without brittle screen scraping.
- Evolve UX without touching business logic every time marketing has an idea.
Without an API-first stance, your white label platform is just another SaaS product with your logo on it.
Real-Time Communication Technologies
Telehealth hinges on latency and reliability, not just “does video work.”
- Video: typically WebRTC-based with TURN/STUN fallback, tuned for low bandwidth and packet loss.
- Messaging: websockets or long-lived HTTP streams to support real-time chat, presence, typing indicators.
- Presence & routing: pub/sub layers for waiting rooms, provider availability, live queues.
The important bit: all of this must be PHI-aware. That means encrypted streams, scoped tokens per session, and hard limits on what metadata leaks to third-party providers. If real-time features live outside the platform’s security model, you’ve just created a compliance side door.
Data Analytics and Reporting
A white label telehealth platform isn’t just about visits; it’s about the data exhaust those visits generate.
Modern stacks typically include:
- An operational store for PHI and live workflows.
- A separate analytics warehouse (redacted or pseudonymized where needed) for reporting and cohort analysis.
- A metrics layer that can answer: utilization, no-show rates, revenue per provider, time-to-appointment, care-path adherence.
Critically, analytics must respect data minimization and access control: not every admin needs raw PHI, but every stakeholder needs trustworthy aggregates.
AI and ML Integration Capabilities
“AI inside telehealth” can be either a toy or a force multiplier, depending on architecture.
Well-designed platforms treat AI as pluggable services, not hard-coded magic:
- In the build layer: AI assistants that scaffold flows, screens, and data models from natural-language prompts.
- In the care layer: AI triage, documentation helpers, eligibility pre-screening, risk scoring — all using PHI-safe patterns.
- In the ops layer: anomaly detection on billing, utilization, or access patterns.
The architectural non-negotiables:
- Clear separation between PHI-touching and non-PHI models.
- Audit trails for AI decisions and suggestions.
- The ability to swap models (vendor A → vendor B) without rewriting the app.
If AI is welded into the core codebase instead of treated as a replaceable capability, you’re one vendor pivot away from a platform rewrite.
Choosing a White Label Telehealth Development Partner
Building a white-label telemedicine app isn’t just about slapping your logo on a dashboard. It’s about creating a branded, compliant digital front door to patient care—without inheriting a mountain of tech debt. That’s why choosing the right partner is everything.

Red Flags in Generic Platforms (Tech Lock-in, Lack of Support)
Let’s be blunt. If a vendor can’t tell you how to migrate off their platform, you’re not buying a solution—you’re buying a hostage situation. Watch out for:
- Tech lock-in disguised as “turnkey simplicity”
- Rigid templates that don’t reflect your patients’ journey
- Slow or outsourced customer service (your team can’t afford delays)
- No real roadmap for HIPAA updates or EHR integrations
And if their devs flinch when you mention Epic or Cerner—run.
Technical Capability Assessment
A white label telehealth partner must prove they can do more than theme a UI. Your due diligence should validate:
- Interoperability maturity — FHIR/HL7 proficiency, event-driven EHR sync, bi-directional workflows
- Extensibility — API-first architecture and modular code that doesn’t trap you in their tooling
- Security engineering — ability to enforce least-privilege, logging, encryption on day one
- SRE/DevOps practices — auto-scaling, uptime SLAs, zero-downtime deploys, monitoring
If the vendor won’t let your engineers speak to their engineers, assume the tech doesn’t hold up to inspection.
Healthcare Domain Expertise
Digital health is where domain blind spots become regulatory failures. A strong partner understands:
- Credentialing flows, licensure rules, payer policies
- Clinical journey design — intake, triage, visit, documentation, billing
- PHI lifecycle — consent, access scoping, retention rules
- Specialty-specific workflows (mental health ≠ urgent care ≠ PT)
Healthcare is a high-context space. Your vendor must speak your language or you’ll pay to educate them — twice.
Support and Maintenance Evaluation
Support determines how fast you recover when production starts throwing curveballs.
Assess:
- Who is responding? (Frontend troubleshooters or compliance-literate engineers?)
- How fast is remediation under operational pressure?
- What’s included in subscriptions — security patches? new features? regulatory updates?
- Is support proactive or purely ticket-driven?
A white label telemedicine platform is a living system. Buying one without proper support is like buying a hospital with no facilities team.
Scalability and Growth Support
A “successful” telehealth launch that breaks under growth is a strategic failure.
This is where you stress-test:
- Horizontal scale capability under Monday-morning peaks
- Region and multi-brand expansion readiness
- Performance isolation between tenants or service lines
- Analytics that can handle thousands of daily encounters — not dozens
Scaling is not a “later” problem. It’s the difference between a pilot and a business.
Contract and Ownership Terms
Sloppy contracts are the most expensive mistake in digital health.
Clarify:
- Does your team own the code? Or only “usage rights”?
- Can you self-host later without a rewrite?
- What happens if you leave the platform?
- Are you locked into a proprietary schema or workflow engine?
If ownership isn’t explicit, assume you don’t own anything — except future invoices.
Reference Customer Analysis
Any vendor can talk a big game. Real questions:
- Do they have live deployments in regulated care models?
- Can you speak to clinical users, not just product sponsors?
- How did they handle:
- go-live stress?
- unexpected integrations?
- compliance audits?
- feature pivots under timeline pressure?
- And the killer question: Would the client choose them again?
If the answer is anything but an immediate “yes,” you have your answer.
What Makes a Partner Like Specode Different
Specode was designed for medical practices that want speed and control. Every component is modular, HIPAA-compliant, and fully customizable—because we focus on what actually improves patient experience, not just design polish.
With us, you get:
- Fast launches (as in under 4 weeks)
- AI-assisted app assembly and continuous iteration
- Full code ownership—no black boxes
- A support team that knows FHIR and ICD-10, not just frontend bugs
And yes, we help you improve patient engagement without bloating your backlog.
Checklist: What to Ask Before Signing the SOW
- Will I own the codebase of this white-label telemedicine app?
- How fast can we go live—with real patients?
- Is this solution compliant out of the box?
- What happens when I need new workflows next quarter?
- How does this compare to the traditional healthcare app development approach?
Launching Your White Label Telehealth Platform
A solid white label stack gets you most of the way there. The launch is where you find out whether you’ve actually built a new clinical channel or just another “pilot we don’t talk about.”
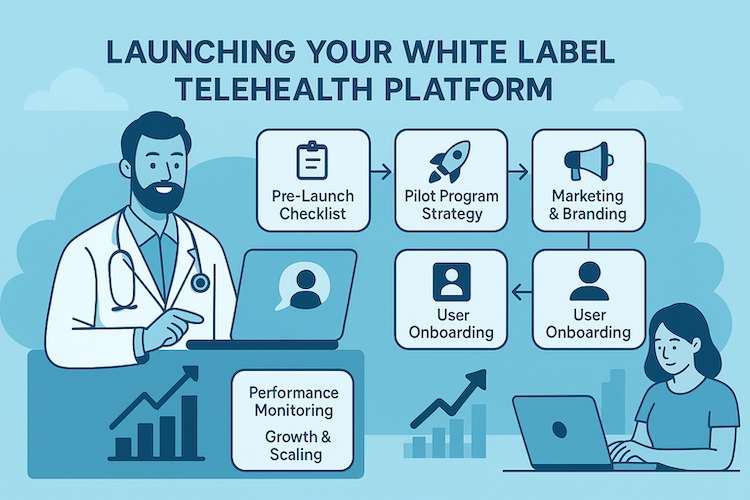
Pre-Launch Checklist
Before real patients touch the platform, three groups need to be aligned: clinicians, operations, and security. Clinicians validate that the full journey works end-to-end; ops confirms staff can actually run that journey; infosec makes sure you won’t be apologizing to the board in six months.
Key checks to have ticked off:
- End-to-end flow runs cleanly: intake → visit → documentation → coding/billing.
- Role-specific UAT for front desk, nurses/MA, providers, and billing.
- Security + backups tested in practice, not just promised in a slide deck.
If these aren’t done, you’re not “soft launching” — you’re stress-testing in production.
Pilot Program Strategy
A pilot is a controlled experiment, not a half-hearted go-live. You deliberately limit scope so you can see cause and effect. Good pilots usually:
- Focus on one specialty, one region, and one primary success metric.
- Run for 4–8 weeks with weekly reviews of issues, workarounds, and edge cases.
- Produce a clear split between “must fix before scale” and “can wait until phase 2.”
The goal isn’t perfection; it’s to prove the model is clinically safe, operationally viable, and worth scaling.
Marketing and Branding Guidelines
Telehealth adoption doesn’t happen just because a login link exists. You need a consistent story across all touchpoints so patients and providers understand why this channel exists and when to use it.
In practice, that means:
- Making virtual care part of the main brand narrative, not an orphaned subpage.
- Using plain language: “video visit with your doctor” beats “synchronous virtual encounter.”
- Giving providers talking points that emphasize efficiency and revenue, not just convenience.
Your white label telehealth platform is your new front door. Market it like one.
User Onboarding Best Practices
Most digital health failures are onboarding failures with nicer UI. Patients need a short, predictable path into the system; providers need to trust it won’t slow them down.
For patients, aim for:
- 2–3 steps: verify → consent → basic context.
- Clear expectations about time, tech requirements, and what happens if something fails.
For providers, keep training tight and role-specific, focused on:
starting visits, finding context fast, documenting efficiently, and getting paid correctly.
Performance Monitoring Setup
If you don’t define success metrics before launch, every complaint will sound equally urgent. A small, well-chosen metrics set will tell you whether to iterate or escalate.
At minimum, track:
- Visit volume, no-show rates, and time-to-appointment.
- Video call success/failure rates and platform error rates.
- Support tickets by type and time-to-resolution.
Dashboards and alerts should exist before go-live. Otherwise, your first monitoring system is just an angry inbox.
Growth and Scaling Strategies
When the pilot stabilizes, resist the urge to “turn it on for everyone.” Scaling is easiest when you change one variable at a time.
A sane scaling pattern looks like:
- Add either more providers, more regions, or more service lines — not all three at once.
- Revisit staffing and workflows with each expansion; telehealth shifts who does what and when.
- Treat every big feature wave (ePharma, RPM, group visits) as a mini-pilot with its own risk check.
That’s how you grow a white label telehealth platform into a durable channel instead of a one-off success story.
Future of White Label Telehealth Platforms
White-label telehealth solutions aren’t a fad — they’re the infrastructure that will support the next wave of healthcare disruption. Here’s how I see that playing out through 2025–2030 and beyond.

Emerging Technologies Integration
Telehealth platforms will soon become hubs for more than video calls and scheduling. Think remote monitoring devices, wearables, IoT health sensors, home diagnostic kits, and embedded tele-pharmacy.
As more of care shifts home — for chronic disease management, preventive care, and remote follow-up — white label platforms must support rapid integration of device data streams, e-prescriptions, patient-generated health data, and asynchronous workflows.
The winners will be platforms that treat integrations as first-class modules — not afterthoughts — enabling organizations to bundle telehealth with RPM or hybrid care without rewriting their stack.
AI and Automation Trends
AI’s impact on telemedicine is accelerating. The market for AI in telehealth & telemedicine is forecast to grow at a ~36.4 % CAGR from 2024 to 2030, reaching ~USD 27.14 billion by 2030.
In practice, that means:
- AI-driven triage, virtual intake bots, automated documentation, and decision support — reducing clinician burden and increasing throughput.
- Predictive analytics for readmissions, chronic-care adherence, and resource-demand forecasting.
- Intelligent automation of administrative workflows (billing, reminders, follow-ups, RPM alerts), making telehealth platforms more efficient, leaner, and lower-cost over time.
In short: white-label platforms with integrated AI will shift from being “a slightly cheaper Zoom + scheduler” to “the operational nerve center” for virtual care.
Regulatory Evolution Impact
As telehealth becomes mainstream, regulatory landscapes will continue to tighten — and evolve. Cross-jurisdiction data privacy laws, reimbursement parity rules, remote care guidelines, and enforcement of security standards will shape the viability of any platform.
For white label telemedicine platforms, this means: platforms must support regional compliance variants, audit-ready reporting, consent workflows, and data residency controls — while remaining flexible enough to adapt as laws change. The next major waves will reward those who embed regulation as core features, not afterthoughts.
Market Consolidation Predictions
The flood of digital health startups and legacy vendors will likely lead to consolidation. Larger health systems, payers, or enterprise platform vendors may acquire smaller white-label providers to internalize virtual-care stack capabilities. This could create two dominant tiers:
- “Platform-as-infrastructure” — large, stable, enterprise-grade stacks powering many downstream brands.
- “Niche vertical players” — smaller, specialty-oriented platforms focused on subsets like mental health, remote monitoring, or chronic care.
For buyers, this underscores the value of code ownership or portability. If you’re locked into an acquired vendor’s roadmap, you might be forced to migrate again — something to vet carefully now.
Innovation Opportunities
Given the convergence of AI, device data, and regulatory pressure, the next wave of innovation will likely come from hybrid care models. Opportunities include:
- Post-acute care at home: video + RPM + e-Pharma + analytics
- Chronic-disease management bundles that combine remote monitoring, AI alerts, tele-visits, and preventive interventions
- Employer/payer-facing virtual care — built under white label but delivered as B2B programs
- Multi-language, multi-region deployments using modular compliance + localization layers
If you architect with modularity and extensibility in mind today, you’re well positioned to capture those opportunities — long before competitors finish a home-grown build.
2025–2030 Market Forecast
Numbers reinforce the long game: The global telehealth market, valued at ~USD 123.3 billion in 2024, is projected to reach ~USD 455.3 billion by 2030.
At that scale and growth rate (~25%+ CAGR), white label platforms that deliver flexibility, compliance, and speed won’t just be alternatives — they’ll become the default foundation for providers scaling virtual care, RPM, and hybrid delivery models.
If you get your architecture, integration agility, and compliance posture right, you won’t be chasing telehealth — you’ll be building the future-proof rails on which it runs.
Why Choose Specode for Your White Label Telemedicine App
If you want the speed of a white-label launch without the rigidity of a one-size-fits-all SaaS, Specode sits in the pragmatic middle: an automated platform with reusable HIPAA-ready components, an AI assistant to assemble them, and full code ownership so you keep control post-launch.
You’re not “locked into a builder”; you’re assembling a production-grade app that your team can extend like any other codebase.
What you get with Specode (in practice):
- Faster launch, real code: AI-assisted assembly compresses timelines by ~30–60% vs legacy builds, while outputting code you own. No blank screens, no boilerplate sprints.
- Healthcare AI builder (chat → live preview): Describe flows in plain English and the assistant assembles screens, data, and permissions on HIPAA rails. Connect your own data early so the UI mirrors real patients/providers/payers; flip on EHR/eRx/labs/insurance integrations. Guardrails (Change Log, role-scoped testing), fully brandable theming, and drop-into custom code—with full code ownership and no lock-in.
- HIPAA-first defaults: Audit logs, role-based access, secure messaging, PHI-safe patterns—baked into components from day one.
- Composable building blocks: Scheduling, telehealth/video, intake & e-consent, patient/provider portals, payments/checkout, notifications, outcomes tracking—mix, match, and customize.
- Integration-ready: Canvas Medical supported case-by-case; Epic/Cerner/athena and other major EHRs via native APIs/middleware; eRx/labs/wearables through partners.
- Code ownership & extensibility: Avoid platform lock-in; launch with Specode’s foundation and keep iterating with your own developers.
- Multi-brand, multi-region support: Localize UI, manage affiliate brands, and scale without re-architecting.
AlgoRX: from Friction-Filled Rx to a “Shopify-Like” Medication Experience
Using Specode, AlgoRX launched a HIPAA-compliant ePharma storefront that automated eligibility, streamlined provider review, and enabled multi-product checkout—turning a traditionally multi-week prescribing maze into a consumer-grade flow.
Outcomes weren’t “nice to have” vanity metrics—they were business metrics: 12× ROI, $1M+ sales by month 2, and 7-figure ARR locked in by month 3.
What shipped (relevant to a white-label telemedicine app):
- Guided onboarding & credentialing for patients and clinicians to keep compliance tight from the first tap.
- eCommerce + questionnaires to capture clinical context inline with checkout (no “we’ll email you later” detours).
- Smart pharmacy routing that respects eligibility, geography, and availability—without slowing the cart.
- Integrated, PCI-compliant payments (NMI) with discounts/affiliate codes for growth levers that don’t break auditability.
- Secure provider–patient chat to resolve clinical questions pre-fulfillment and cut abandonment.
- Admin & analytics to manage meds, providers, and workflows from one pane—so ops can scale with demand.
“They delivered on the exact day… product far exceeded expectations… hired them for ongoing support.” — Adam Hotchkiss, Co-founder, AlgoRX.
Bottom line: with Specode, “white label” doesn’t mean cookie-cutter. You launch fast on a HIPAA-ready foundation, keep your brand and your code, and integrate the clinical/payment stack you already rely on—without duct tape.
Ship a branded, HIPAA-ready MVP fast — start with the AI builder, free.
Let’s make sure your platform delivers quality care without reinventing the wheel.
Frequently asked questions
They’re often used interchangeably, but technically, private label implies exclusive branding rights; white label may be sold to multiple customers with separate branding.
Yes, if you want a professional, branded platform without building from scratch. Just make sure it doesn’t overcomplicate your workflows.
Specode projects typically start at $30K for an MVP. Pricing depends on complexity and integrations.
Yes. Specode supports custom EHR integrations, including Epic, Cerner, and region-specific systems.
Between 4-6 weeks in most cases, thanks to pre-built components and AI-assisted assembly. However, it depends on the level of customization you may need.
With Specode, you get healthcare-savvy support—real humans who know HL7, not just helpdesk scripts.
Absolutely. Our platform was built for multi-brand, multi-region growth with modular add-ons and no vendor lock-in.









