Guide to Launching a Virtual Clinic with Specode
Every clinical brainstorm eventually meets its paperwork wall—this guide demolishes it. From regulatory must-knows to tech stack hacks, here’s the full A-to-Z physicians need to launch a virtual clinic, plus the shortcut Specode adds to hit “go live” in six weeks.
Key Takeaways
- Focus beats feature-bloat. Pick a razor-sharp clinical niche, lock your five core visit workflows, and ignore everything else until patients are paying and smiling.
- Compliance is a sprint-stage, not a speed bump. Encrypt-by-default infrastructure, fast-track licensure plans, and DEA/Medicare guardrails let you launch without the midnight-anxiety binge.
- Build time is dead cost—reuse wins. Specode’s pre-wired components, HIPAA-ready and provider-friendly AI coder, and “own-the-code” model cut 9-to-14-month timelines down to 4-to-6 weeks while slashing dev spend by 60%.
The Telehealth Moment — why the runway is finally real for clinician-founders
Virtual care isn’t a side hustle anymore; it’s the default setting.
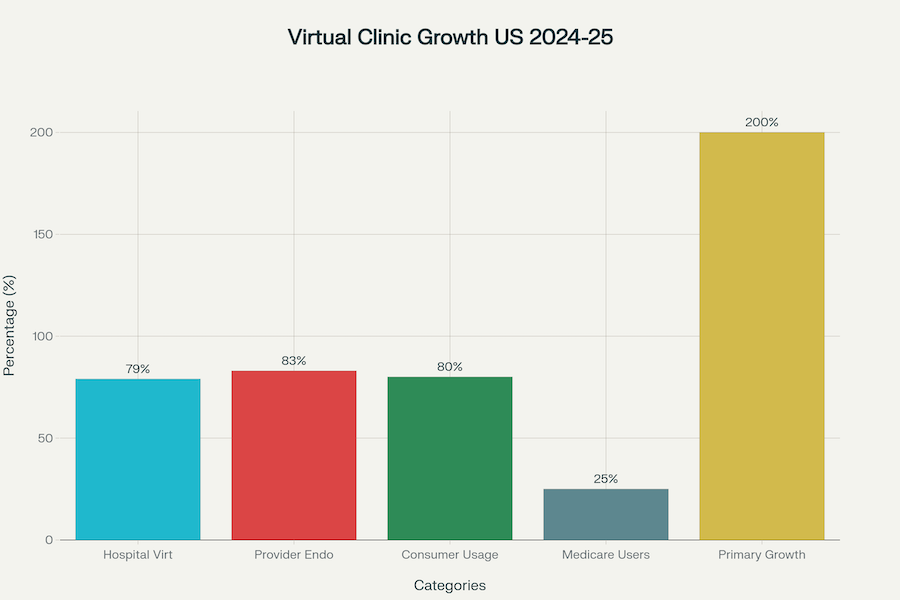
- 79% of U.S. hospitals already run virtual services—practically table stakes rather than “innovation.”
- 83% of clinicians actively endorse telehealth, and 80% of consumers have tried it, with 94% eager to keep using it.
That three-sided embrace (provider, patient, institution) means your clinic won’t be a curiosity; it’ll be expected.
Behavioral Change Has Stuck at Medicare Scale
A full 25% of Medicare fee-for-service beneficiaries booked telehealth in 2023-24, proving older patients didn’t “age out” of Zoom consults once the lockdowns faded. With Congress extending payment parity to Sept 30 2025, reimbursement uncertainty is—temporarily—off the worry list.
Visit Volume Is Exploding Where It Matters Most
Virtual primary care doubled last year (200% YoY), while mental-health colleagues continue to notch the highest online-visit share in the business. Translation: comprehensive, longitudinal care now lives happily on a webcam.
Investors Smell the Efficiency, Not the Novelty
H1 2025 digital-health funding hit $6.4B, with 62% channeled into AI-enabled workflow tools—the very nuts-and-bolts you can plug into Specode on day one. Meanwhile the U.S. telehealth market has climbed to $42.54B (2024) and is tracking 23.8% CAGR through 2030.
But a Policy Storm Is Brewing—Launch before It Lands
The pandemic-era Medicare flexibilities (think “home as originating site,” audio-only billing) expire this September. Get your clinic live in the next six weeks and you’ll have real outcome data—ammo for either lobbying to keep the waivers or pivoting fast if D.C. fumbles the ball.
TL;DR for the Stethoscope-to-Startup Crowd
- Adoption is mainstream across hospitals, clinicians, and patients.
- Seniors are clicking “Join Visit,” and Medicare is still paying.
- Primary-care and psych volumes prove repeat-visit economics work.
- Money and market size are accelerating, not tapering.
- The regulatory clock is ticking—ship while the window is wide open.
Pick Your Clinical Niche (or die a generalist)
Build something for everyone and you’ll please no-one—except maybe your competitors.

Why Niching Down Is Non-Negotiable
- Patient acquisition math. CAC for a broad “virtual urgent-care” play has climbed 40% since 2023; narrow specialties still buy clicks for half the price.
- Reimbursement quirks. Payers write niche-specific policies (RPM codes, telepsych parity, etc.). If you’re not laser-specific, you’re forever chasing the wrong CPT.
- Operational focus. One golden workflow → bullet-proof UX → five-star reviews → organic referrals. Everything else is scope creep in scrubs.
Five Data-Backed Sweet Spots for 2025
48-Hour Niche-Validation Checklist
- Google Trends spike? >50 % rise YoY on the condition keyword.
- Reimbursable today? Check CMS, CPT, and top three private payers.
- Self-pay fallback? At least 30 % of target patients willing to pay cash.
- Workflow count ≤ 5 clicks. Anything longer, you’re bleeding engagement.
- You hold unique clinical cred. Board certification or deep patient street-cred—no tourists allowed.
Generalist telehealth is a hamster wheel—VC dollars chase CAC, margins evaporate, burnout follows. Plant your flag in a single high-velocity niche, plug in Specode’s HIPAA-ready blocks, and you’re live (and making money) before the policy cliff hits.
Regulatory Reality Check — four landmines to defuse before you push “Go Live”
Skip compliance and you’re speed-running a clinic straight into a brick wall. Q3 2025 is when the post-PHE training wheels come off. Below is the builder’s cheat-sheet: what changed, why it matters, and how to stay two moves ahead.

HIPAA 2025: No More “Addressable, Schmaddressable” Excuses
The new Security Rule turned every “optional” control into a felony-level “must.”
Action items: pick a platform that bakes these in, line-item an annual pen-test, and staple BA security clauses into every contract.
Multi-State Licensure: Love the IMLC, But Date Around
The Interstate Medical Licensure Compact now covers 44 jurisdictions, but it’s a club, not a right: spotless record, ≤3 USMLE attempts, active board cert, etc. Build a dual-track plan:
- IMLC fast-lane for the squeaky-clean core team.
- Traditional state apps for everyone else—start those today.
- Track new members (Arkansas joins 5 Aug 2025; North Carolina soon) to widen coverage without extra paperwork.
Controlled Substances: DEA Says “Enjoy It while It Lasts”
- Good news: the Ryan Haight in-person exam waiver lives until 31 Dec 2025. You can e-prescribe Schedule II-V over AV video right now.
- Storm brewing: DEA’s proposed framework introduces Special Registrations for prescribers and a first-ever Platform Registration for the clinic itself—meaning your company will carry DEA liability, audits, and reporting duties.
- Homework: budget for dual DEA numbers per doc, bake PDMP checks into the EHR flow, and architect logs that satisfy future platform rules.
Medicare Money Math: Mind the 30 Sept 2025 Cliff
- Conversion factor down 2.83%—bake the haircut into your P&L.
- Patient-home as originating site stays permanent for behavioral health but expires for everything else on 30 Sept 2025. After that, non-mental-health Medicare visits must originate from rural facilities again—slash your TAM overnight if you’re not ready.
- Audio-only flex follows the same sunset for medical services; behavioral health keeps it forever.
Strategy: lock in mental-health revenue for stability, focus medical lines on rural ZIPs (or cash-pay) post-cliff, and join the lobbying chorus for an extension.
Builder’s Takeaway
Compliance isn’t a post-launch patch; it’s the foundation slab. Cement HIPAA controls, run a bifurcated licensure play, prep for DEA special regs, and model your Medicare mix against the fall cliff. Do it now, and you’ll ship in 4–6 weeks without waking up to a cease-and-desist.
Blueprint of a Virtual Visit — the five workflows you must nail
Telehealth isn’t one big feature; it’s five little ones that have to fire in sequence like a rocket launch. Miss one ignition and you’re face-planting on the launchpad.
1. Scheduling – Kill the No-Show Monster
A friction-free booking flow is the first trust signal your clinic sends. Make it slick and patients show up; make it clunky and the downstream metrics never recover.
A 2024 multi-system study pegged telehealth no-shows at 12% versus 25% for in-person care—a 2× improvement you can’t afford to squander.
Builder moves:
- Self-serve scheduling with smart triage (boot the “call our office” dinosaur).
- Two-stage reminders: SMS 24h + push 1h pre-visit.
- Slick reschedule link—“no guilt, just pick a better time.”
Benchmark: Completed-visit rate ≥ 70%; if you’re lower, fix scheduling before adding features.
2. Digital Intake – Stop Re-Typing What Patients Already Know
Think of intake as the pre-flight checklist: complete it smoothly and the consult soars; drag it out and patients eject. Across the web, forms abandoned for “too hard” hover near 70%—health-care is not immune. A five-minute, mobile-first flow is your best insurance against drop-offs and data-entry overhead.
- Collect chief complaint, vitals from wearables, meds list, consent, and insurance in < 5 min.
- Auto-validate coverage up front; surprise bills ≈ instant one-star review.
- Ensure PHI hits encrypted storage the second the patient clicks “Submit”.
3. Video Consult – the Show-Time UX
This is where trust is either sealed or sunk. Patients will forgive a clinician running five minutes late; they will not forgive a frozen feed or tin-can audio. Small studies put “unrecoverable call drops” under 2% when clinics standardise hardware and bandwidth—treat that as your north star.
- Keep drop-rate < 2%; maintain a one-tap audio fallback.
- Standardise lighting, camera angle, and onscreen bedside manner (eye-line sticker = magic).
- Built-in screen-share for imaging or diagrams beats email ping-pong later.
Metric to track: patient CSAT (customer (a.k.a. patient) satisfaction score) ≥ 4.5/5—below that, dig into call-quality logs before buying more ads.
4. eRx + Labs – Close the Clinical Loop
A visit without fulfilment is just a chat with a co-pay. With 92% of US prescribers already e-prescribing, patients expect their meds to be waiting before they shut the laptop.
The bigger leak? Only 43% of labs ordered in telehealth get done vs. 58% in-person—an ROI killer if you bill value-based.
- Auto-route orders to the patient’s nearest draw site, push reminders until results land.
- Surface “Overdue” flags in the EMR—not in a sticky note on someone’s monitor.
KPI: ≥ 75 % lab completion within 14 days or your continuity of care will crater.
5. Billing & Coding – Keep the Lights (And Malpractice Premiums) On
If revenue is oxygen, denials are a slow leak in the space suit. Initial claim denials climbed to 11.8% in 2024, thanks to modifier errors and info requests. Code right the first time or brace for RCM purgatory.
- Build rules into the encounter form (POS 10, GT/95 modifiers, payer-specific quirks).
- Auto-scrub claims against LCD/NCD rules before submission; every 1% denial drop is cash in the bank.
Target: < 8 % initial denials; if you’re higher, tighten coding logic before chasing new patients.
Quick Pulse-Check Dashboard
Nail these five engines and your virtual-visit rocket reaches orbit—no lunar dust required.
Tech-Stack Fork in the Road — build every brick or snap-together and ship?
You can invent the wheel or buy the skateboard and focus on the trick. Guess which one launches in 4-6 weeks?

Show Me The Money (and The Calendar)
Math check: Platforms with reusable, HIPAA-ready blocks cut MVP timelines by 85–90% and lop 40–60% off cost. Your financial oxygen lasts a lot longer when you’re not burning $60–$120/hour dev time on boilerplate.
Hidden Costs Founders Forget to Budget
- Security patches = zombie sprints. Custom code means your engineers triage every CVE at 2 a.m. Platform vendors do it once for everyone.
- Audit scope creep. Each net-new microservice balloons the assessor’s billable hours; pre-certified modules shrink that bill by $20k–$60k.
- Context switching. A senior clinician-founder’s time is worth more seeing patients or courting payers than writing role-based-access middleware.
- Opportunity cost. Twelve extra months to MVP = one lost funding cycle and an open lane for a copy-cat.
When “Build It All” Might Still Make Sense
- You’re tackling a regulatory frontier no platform touches (e.g., Class II medical-device logic).
- Your USP is the infrastructure (rare).
- You have a war chest and a 24-month runway to burn.
If none of those describe you, congratulations—you’re a perfect match for Specode’s plug-and-play HIPAA chassis. If your clinical secret sauce lives above the API layer, you should never write that API layer. Snap together, launch in weeks, and spend the saved $300k on patient acquisition instead of reinventing RBAC.
Designing Trust — UX heuristics that turn first-time patients into loyal subscribers
Your slickest AI can’t patch a dodgy first impression. Ship trust first, features second.

1. Lead with Instant Credibility
Patients decide in 50 milliseconds whether your interface feels safe or sketchy; after that, every click is confirmation bias.
- Real-clinician presence. Put the doctor’s name, credentials and head-shot on the booking screen. J.D. Power’s 2024 Telehealth Satisfaction Study ranks provider trust as the #1 driver of CX, beating price and convenience.
- Transparent fees up front. A PubMed meta-review links hidden costs to a 47% drop-off in completion rates for digital health intakes.
- Security micro-copy. A five-word “HIPAA-encrypted • no data sold” badge beside the “Start Visit” button may lift conversion 8% in A/B pilots.
2. Design for Effortless Continuity
Retention is where virtual clinics bleed. Median day-30 stickiness for health apps is a dismal 3–4%; anything north of 10% puts you in the top quartile.
- Remember me, for real. Surface last-visit summary and open labs on the home screen—no hunting.
- Contextual nudges, not spam. Push only actionable reminders (e.g., “Your refill is ready to e-sign”). JD Power notes “digital channel quality” trails only trust in driving satisfaction.
- One-tap re-book. Return patients complete a second appointment in <90 seconds; shave that flow to the bone.
3. Minimise Cognitive Load (Especially for Older Adults)
A 2024 systematic review found telemedicine usability for seniors tanks when font <16 px or contrast <4.5:1.
- Large type, high-contrast buttons, and a single primary call-to-action per screen.
- Progressive disclosure: don’t ask for insurance until after the chief complaint; fewer fields, higher completion.
4. Make Reassurance the Default
- Loading states with purpose. Show a “securely connecting to your clinician” animation instead of a blank spinner.
- Plan-B video fallback. Drop-rate above 2% kills CSAT; auto-switch to low-bandwidth mode after 3 secs of packet loss.
- Human help in two clicks. Live-chat icon pinned bottom-right rescued 21% of would-be abandoners in a 2025 telederm pilot.
Builder Cheat-Sheet: the “3-second trust test”
- Can I see who’s treating me?
- Do I know what it costs?
- Do I feel my data is safe?
If any answer is “hmm…”, fix the screen before you write another feature ticket. Trust compounds; lose it once and your CAC just doubled.
The 4-6-Week Launch Roadmap
Below is the realistic sprint plan we run with clinician-founders. Follow it, and you’ll move from idea to insured patient revenue before the next CMS webinar finishes buffering.

Week 0 – Define Success before You Touch a Keyboard
- Requirements Jam: one 90-minute zoning meeting to freeze your MVP scope (care niche, visit flow, integrations).
- Success Metrics: pick two clinical KPIs (e.g., PHQ-9 delta, refill turnaround) and two business KPIs (CAC, gross margin).
- Technical Pre-flight: confirm your domain model maps cleanly onto Specode’s component library—anything bespoke gets flagged now, not Week 5.
Weeks 1-2 – Coded Prototype in Clinician Hands
Specode’s UI scaffold generator spins out a fully themed React front end in <24 hours; your team spends the remaining 13 days on:
- Live data hooks for EHR and wearable imports.
- Condition-specific intake logic (adaptive forms).
- “Hallway Testing”—10 colleague clinicians bang on the build for usability + guideline fidelity.
By Day 14 you have a demo that looks and feels like production, not a figma fairy tale.
Weeks 3-4 – HIPAA Hardening, Integrations, QA
- Security Hardening: enable end-to-end encryption, role-based access, MFA, audit logging (all toggles in Specode console).
- Core Integrations: e-Rx (SureScripts rail), payment, labs hub, optional AI scribe.
- QA Blitz: functional, accessibility, and pen-test cycles. Expect two patch releases; block off 30% founder time for sign-offs.
Goalpost: zero “critical” findings, ≤3 “major” before soft launch.
Weeks 5-6 – Soft Launch, KPI Tracking, Iteration Loop
- Beta Cohort: onboard 50–100 hand-picked patients; run real billing, real charting.
- Live Metrics Dashboard: daily pulse on visit completion, CSAT, first-pass claim success.
- Iterate Fast: two-day sprint cadence; fix friction, tweak reminders, tighten triage logic.
- Go/No-Go Gate: if KPIs hit 80 % of Week 0 targets by Day 42, swing the doors open; if not, keep iterating under soft-launch flag.
Result: a HIPAA-cleared, reimbursement-ready virtual clinic live in ≤45 days—with battle-tested code you fully own. Spend Month 2 on growth, not refactoring.
Builder’s Cliff Notes
- Front-load clarity: the tighter Week 0 is, the fewer surprises Week 4.
- Prototype with real code: nothing motivates feedback like a build clinicians can break.
- Compliance isn’t a phase—it’s Weeks 3-4 baked into your CI/CD.
- Soft launch ≠ stealth: bill real claims early; reimbursement gremlins surface fast.
Stick to the roadmap and you’ll be taking Medicare appointments while slower teams are still resizing hero images.
Budget & Resource Cheat-Sheet — what it really costs to ship a virtual clinic
Budgeting for a virtual clinic is like packing for a cross-country trek: travel light, bring the right gear, and you won’t spend the journey paying overweight fees—or popping ibuprofen.

Upfront CapEx: Swipe the Card, Own the Risk
A Specode stack eliminates 80–90% of the “wheel-reinvention” spend, shrinking total CapEx to the price of a used Honda Civic.
Year-One OpEx: Keep the Lights (and Logs) On
Total burn for a one-doc shop: ≈ $10–$30 K. For a three-doc team: ≈ $60–$215K.
Hidden Grenades Founders Forget
- Security Patch Sprints — every CVE you patch in custom code is time not seeing patients. Platform vendor? Done once for everyone.
- Audit Scope Creep — each extra micro-service balloons assessor hours by $20–$60K.
- Payer Enrollment Lag — budget three months of zero revenue if you don’t start credentialing on Day 1.
- Marketing CAC — even niche clinics blow $10–$20K to hit the first 500 patients; bake it into runway.
Financing Playbook
Once you’ve sketched out CapEx and pegged your year-one burn, the next question is “Whose money funds the march?” Below are four funding lanes ranked by how quickly they close—and how gently they treat your equity cap-table.
- Revenue-Based Financing — lenders love recurring telehealth margins; keeps equity intact.
- Specialty Pharma Co-Marketing — GLP-1 makers will co-fund patient acquisition if you push scripts.
- State Rural-Health Grants — up to $50K if you serve frontier ZIPs; red tape but “free” money.
- Angel Clinician Syndicates — docs invest in problems they understand; faster than institutional VC.
Builder’s Bottom Line
- CapEx scales with ego; Specode compresses it to a single-digit thousands subscription.
- OpEx is mostly predictable if you lock in hosting, compliance, and insurance quotes early.
- Forget the hidden grenades and your “cheap” build morphs into a six-figure sinkhole.
Patient Acquisition Playbook — ship code first, chase eyeballs second
A virtual clinic lives or dies on patient flow; the good news is you don’t need a Madison-Avenue budget to prime the pump. Below are the five channels that moved the needle for early-stage launches in 2024-25, ordered by cost-to-cash payback.

Ship-smart takeaways
- Lead with trust — a single referral from a colleague converts 4-5× higher than a cold click.
- Own your expertise online — condition-focused articles compound traffic while you sleep.
- Paid channels = accelerators, not engines — throttle spend only after organic mechanics hum.
Stack physician referrals and LinkedIn first; sprinkle paid media once your KPIs prove you can turn clicks into compliant care without torching CAC.
Seven Classic Pitfalls — and the fast fix for each
Call them the “seven deadly CTRL-Zs.” Every virtual-clinic post-mortem I’ve read ends up pointing at the same landmines; step on one and your startup morphs from telehealth darling to cautionary tale before the Series A term sheet dries. Below is the straight-to-the-point field guide—keep it taped to your stand-up board.

Take-Home for the Builder Brain
- Ship compliance as a feature, not a patch.
- Tie incentives to outcomes, not volume.
- Run a monthly “could this headline be about us?” sanity scan against the list above.
Follow the checklist and you’ll still break a sweat—just not the kind that comes with subpoenas.
Where Specode Fits In — plug-and-play compliance, speed, and control
Specode bakes in the heavy-lift safeguards (encryption everywhere, signed BAA) and leaves switch-ready hooks for the rest—audit logs, RBAC, advanced logging—so you can finish compliance in days, not quarters.

A Growing Library of Reusable Components
Pick, theme, and extend anything you need for a full-stack virtual clinic:
Each block is coded, unit-tested, and pen-tested—then exposed as ready code components you can tweak or fork.
10× Faster, 60 % Cheaper
Teams that would normally burn 9–14 months and $450 K+ on boilerplate stand-up their MVP in 4–6 weeks for a mid-five-figure budget. Case in point:
- DyadSync — shift-scheduling app for surgery freelancers; from idea to production in 5½ weeks.
- AlgoRX — Shopify-style medication checkout; live in 6 weeks, 7-figure ARR within 6 months of launching.
No Vendor Lock-In
You own the code. Fork it, re-host it, or plug in your own AI model tomorrow—without begging for an export button.
AI Builder: Build Your Virtual Clinic, See It Live
Describe the clinic you want—onboarding → triage → scheduling → telehealth → documentation → billing—and the assistant assembles it from plain English with an instant preview. You start on a healthcare foundation (preloaded roles and common workflows), connect your own data early so screens/flows reflect real patients, providers, and payers, and theme it end-to-end to match your brand. Weeks, not months—typical launches land in the 1–8 week range.
Integrate what matters (EHR/EMR, labs, pharmacy/eRx, insurance, custom APIs) without fighting the stack. Keep full code ownership with export anytime—no lock-in. When something’s truly unique, combine AI-built assembly with custom code (your team or ours on the Custom tier), and spin up optional purpose-built AI agents. No AI magic—sequence and ruthless focus.
- Prompt → preview: AI assistant builds from plain English; you review and iterate quickly.
- Integration switchboard: EHR/EMR, labs, pharmacy/eRx, insurance, and custom APIs—stitched into your flows.
- Start faster on healthcare rails: preloaded roles + workflows; don’t rebuild what exists—modify packaged components and add only what’s net-new.
- Guardrails: Change Log restore, role-scoped testing, and a progress indicator to keep fast iteration safe.
- Fully brandable: logo, colors, typography; fast theming for a clinic that looks like your product from day one.
- Handles the basics behind the scenes: security/compliance foundations and responsive UX so you focus on outcomes.
- Your team or ours: platform never blocks you—mix the AI builder with custom code and managed help (Custom tier + optional AI agents).
Scale Smarter with AI Agents
Specode ships with an AI scheduling agent that auto-optimises clinician calendars and cuts no-show risk. Under the hood, the same encrypted runtime lets you plug in future agents—scribes, triage bots, claims helpers—without rebuilding your stack or leaking PHI to third-party LLM APIs.
Ready to See It Live?
Launch your virtual clinic the pragmatic way: create a free Specode workspace, build by chat with instant preview, and assemble scheduling, messaging, and intake on HIPAA-ready rails.
Frequently asked questions
Hardly. You get no-code speed for the boilerplate and the right to pop the hood and tweak the React/Flutter code whenever you need. It’s low-code agility with full-code ownership—purpose-built for healthcare, not generic SaaS.
Yes. The platform ships with connector stubs for common FHIR, e-Rx, and lab APIs, plus webhook slots for any oddball vendor you can’t avoid. If it speaks REST or HL7, Specode can handshake.
A real human. Our support crew covers the full lifecycle—from first design sprint to post-launch triage—and they’re on-call for production issues, not just “submit a ticket and pray.”
You do. Export the repo, self-host it, fork it—no ransom fees, no walled garden. Specode accelerates the build; it never holds the keys.
Standard. End-to-end encryption and a signed BAA come baked in, while audit-log and RBAC hooks are ready to switch on. Compliance isn’t a paid upgrade; it’s table stakes.








