Patient Intake Management App Development Guide: Where Adoption Meets ROI
Most digital patient intake rollouts don’t fail on features—they fail on muscle memory. If your team still reaches for clipboards after go-live, you don’t have a software problem; you have a workflow takeover problem. This guide shows how to fix adoption, model ROI, and architect integrations that won’t haunt your audits.
Key Takeaways
- Adoption beats features: map real workflows, ship EMR write-back and data validation on day one, and run parallel for two weeks—otherwise you’re buying double entry with prettier fonts.
- Strategy > price: in patient intake app development, buy when intake is table stakes; assemble/customize with a HIPAA-ready healthcare AI builder and drop to custom code only where intake logic is your moat (data reuse, multi-system orchestration).
- Architecture prints money (or burns it): define ownership, idempotency, and audit trails; when intake captures structured medical history and runs a symptom checker to route care, you’re building leverage—not just forms. Use an AI builder on HIPAA rails to compose intake → triage → routing → EHR write-back without rebuilding plumbing.
Why Most Intake Implementations Miss the Mark
A regional ortho practice drops $30k on a shiny new intake platform. Demos were impressive. Features check every box. Six months post-launch, the front desk is still handing out clipboards. The system? Collecting dust behind a forgotten login screen.
Here’s the brutal irony: 92% of patients are willing to complete digital forms for convenience and accuracy. Patient demand isn’t the problem. So why do implementations crater?
Reality Check from the Trenches
Case in point: clinics that roll out digital forms without EMR write-back force staff to re-key every field—double work, zero time savings—so teams quietly route patients back to paper. That pattern is widely reported in implementation post-mortems (“twice the work” when staff keep documenting on paper), and in one published clinic case, moving to integrated forms with EMR write-back cut duplicate entry and halved check-in time.
The Adoption Paradox, in Numbers
Feature-rich systems—conditional logic, e-signatures, insurance verification, mobile flows—still struggle to mesh with real healthcare workflows. The data backs it up:
- Patient appetite is real: between 77% and 92% want to finish pre-visit questionnaires; yet across 6,300+ practices, median digital engagement sits at ~14/100. That’s not a features problem; it’s a workflow problem.
- 42% of healthcare software buyers say staff acceptance & training is the #1 implementation challenge. Translation: if the intake workflow fights muscle memory, muscle memory wins.
- Count the failures honestly and the rate climbs: up to 70% of tech transformations miss their goals when you include delays, overruns, or abandonment—healthcare is not exempt.
The bottleneck isn’t the software. It’s the friction between entrenched habits and the new intake workflow. Staff who’ve perfected a clipboard-to-EHR routine aren’t “anti-tech”—they’re protecting a process that actually ships work.
When training is rushed, documentation unclear, or the handoff to scheduling breaks, teams revert. In partial rollouts, staff often keep documenting on paper—twice the work—torching administrative efficiency and patient experience.
The real insight? Intake isn’t a software problem—it’s a workflow takeover problem. Treat choosing a patient intake management app as a process-redesign initiative, not a procurement checkbox. Concretely:
- Map the current state before configuration. Identify every handoff across patient flow, healthcare workflow, and patient management solutions.
- Build muscle memory with parallel runs. Two weeks of side-by-side beats a one-hour lunch-and-learn.
- Ship integrations, not promises. Prioritize EMR write-back on day one; it’s the difference between adoption and polite sabotage.
Frame the decision correctly and you stop shopping for features and start designing an intake workflow that your team will actually use—improving patient flow and administrative efficiency without mortgaging clinician goodwill.
Practices that nail this don’t start with demos; they start with a workflow audit, staff input, and a vendor willing to iterate past go-live. That’s how you win with digital patient registration.
The Build vs Buy Decision Framework for Health-Tech Founders
Patient intake software isn’t a pure cost line; it’s a strategy call. The real question isn’t “What’s cheaper?” It’s “Where does intake sit in my competitive advantage stack?”
The Decision Tree That Actually Works
Buy signals (off-the-shelf patient intake platform):
- Your intake workflow mirrors standard ambulatory patterns and existing practice management tooling.
- Integrations are light (demographics + scheduling); a generic form builder with e-signature is “good enough.”
- Speed > differentiation (you need something live in 30 days); small team means limited bandwidth for maintenance.
Build signals (custom intake):
- Proprietary clinical intake that competitors can’t easily copy; custom forms with branching/eligibility logic that drive revenue or outcomes.
- Evented data hooks that trigger downstream rules (eligibility, routing, orders) in your EMR/ops stack.
- Multi-location coordination and complex coverage/cost flows that shape patient experience and ops.
The Real Cost Math
Here’s where budget conversations go sideways. Off-the-shelf systems often land around $300–$800+ per month depending on panel size and features—roughly $3,600–$10,000+ annually for established solutions; larger orgs with complex needs can exceed that quickly. Custom builds? A focused intake MVP typically falls in the $50,000–$70,000 range, with 15–25% annual upkeep.
The trap is comparing year-one SaaS ($8k) to custom ($60k) without pricing the compliance debt and rework tax when your intake can’t handle the eligibility logic or branching that underpins your model. Eighteen months later, you “buy again”—after burning time, losing signal in your data, and denting margins and velocity.
Sanity check: if intake is 10% of your value prop, buy it. If it’s 40%+—the engine for differentiation—build it (ideally by assembling proven, HIPAA-ready modules vs. a blank IDE).
When Intake Becomes Strategic
AlgoRX hit this exact fork. They needed intake tied to eligibility screening, provider automation, and pharmacy routing—essentially a Shopify-style checkout for medications. No off-the-shelf form builder could support the branching rules (BMI gates, state restrictions, contraindications) plus real-time provider automation and eRx.
Assembling with modular components (dynamic questionnaire → provider workflow → pharmacy routing) delivered the goods:
- 7-figure ARR by month six
- a measured 15× ROI
Why it worked: intake wasn’t “just forms.” It orchestrated end-to-end healthcare workflow—from structured eligibility capture to provider approvals and pharmacy fulfillment—boosting throughput while preserving compliance. That’s the distinction between commodity patient intake software and a defensible intake engine.
Use off-the-shelf when intake is table stakes. When intake is the moat, assemble—so you keep speed and control over the parts that actually move revenue and experience.
What Actually Drives Patient Completion Rates
Completion rates aren’t a fixed number—they’re a verdict on your implementation. The same flow can clear above 70% with clean UX and sequencing or sink below 50% when friction stacks up. Same platform, opposite results—sequencing and micro-friction decide completion.
Three Conversion Killers
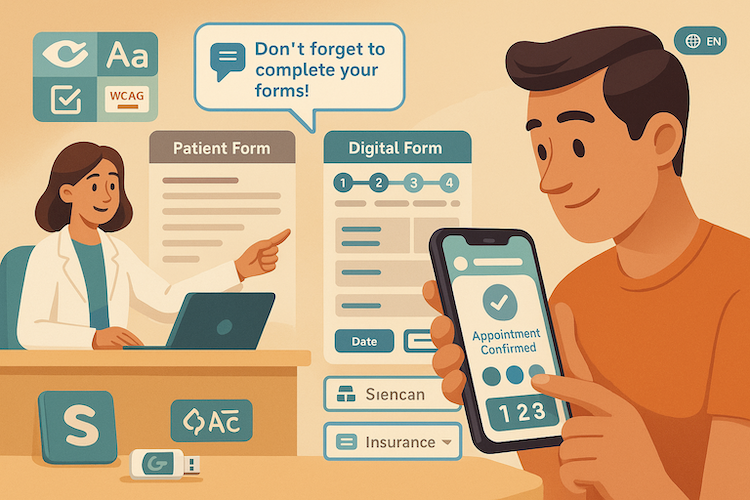
- Thumb-hostile mobile UX. Inputs that fight rather than guide (tiny targets, jumpy focus, no numeric keyboards) tank patient engagement during mobile check-in.
- Bloat posing as diligence. Long patient forms and catch-all medical questionnaires signal, “this will take forever.” Trim ruthlessly.
- Weak confirmation moment. If it’s not clear the appointment locks on submit, people assume their effort was wasted.
Fields vs. Sequence
- It’s not “how many fields,” it’s which ones, when. Phone number requests are classic friction—multiple experiments show meaningful drops when you ask too early (e.g., –48% in one case). Push sensitive asks later or collect in visit two.
- Progressive intake beats “everything upfront.” Capture minimum viable data (name, insurance, chief complaint) first; pull the rest from referrals, eligibility, or prior digital forms. Pre-populate wherever possible—perceived seconds saved matter.
For digital patient intake, design the flow the way patients work, not the way org charts look: short steps, tight defaults, obvious next actions.
Structure the Form for Momentum
Multi-step > single-page for anything beyond a dozen inputs. Expect meaningfully better completion (reported lifts from +14% to +86% depending on context), largely because smaller steps feel lighter and allow conditional logic so people only see what’s relevant.
SMS and email nudges help recover a real share of abandons; SMS has widely reported ~98% read rates, and randomized studies show text reminders reduce no-shows—use that same muscle for completion prompts. Keep messages short and specific.
Don’t Forget the Basics That Compound
- Accessibility (labels, contrast, error hints, focus order) and multi-language support—both are table stakes that directly affect completion and patient onboarding quality.
- If you’re packaging this into a medical forms app, expose sensible defaults (date pickers, insurance picklists) and mirror real-world accessibility constraints (assistive tech, timeout logic).
Takeaway: Completion is an outcome, not a feature. Ship mobile-first simplicity, sequence only what’s necessary, use conditional branching and gentle rescue flows, and you’ll turn abandonments into throughput—exactly what you want from a patient intake form app.
Integration Architecture That Doesn’t Accumulate Debt
The “integration tax” isn’t mysterious—it’s where 3–6 months quietly disappear. The culprits are predictable: identity matching (MRN vs portal IDs), auth and token scopes, eligibility round-trips, vendor rate limits, and UAT queues that move at clinic speed, not sprint speed. Price the work you can’t demo: retries, reconciliation, and observability.
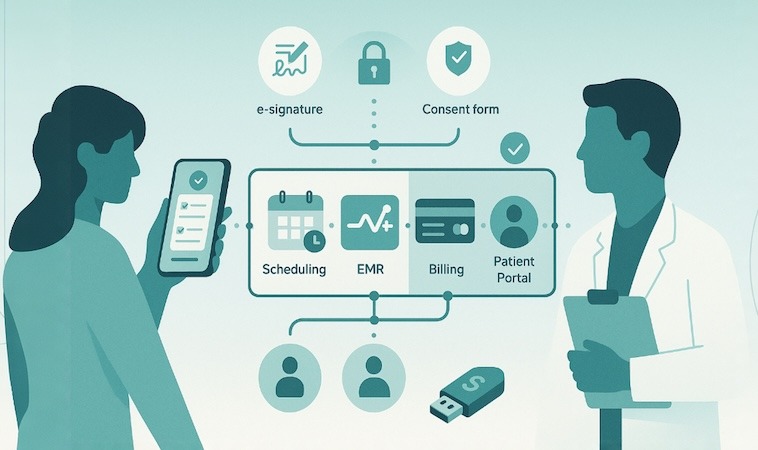
Data Ownership Map
- EMR owns demographics, insurance, clinical flags.
- Scheduling/PMS owns availability and constraints for appointment scheduling.
- Intake owns draft state only (TTL on drafts; purge rules).
- Logging is PHI-safe (structured redaction, no free-text PHI in logs).
Where Implementations Actually Break—and the Fix
- Demographics drift → use idempotency keys and versioned upserts; never “append” identity.
- Insurance verification loops → make eligibility checks asynchronous with visible status + exponential backoff; show real-time updates to staff and patients.
- Consent form versioning → immutable versions with a signed hash; link consent to encounter/audit so billing/compliance can be reconstructed.
- Patient portal edits → treat portal updates as first-class events; apply conflict policy (see below) instead of silent overwrites.
Working Patterns
- Outbox/inbox + DLQs so transient vendor failures don’t become lost writes.
- Event catalog with contracts: Intake.Submitted, Intake.Amended, Intake.Signed, Scheduling.SlotHeld, Payment.Authorized.
- Conflict policy: last-writer-wins for non-clinical fields; route contested clinical data to a review queue.
- Observability SLIs: successful write %, submit→EHR integration latency, max staleness window. Gate cutovers on SLOs, not vibes.
In the middle of all this, your patient intake management system should behave like a message-driven service that pre-populates, validates, and hands off cleanly—owning the draft, not the truth.
FHIR/HL7 Reality Check
Not every system speaks clean APIs. Expect partial FHIR, custom extensions, polling in place of webhooks, paging limits, and $everything timeouts. Keep a fallback ladder: FHIR → vendor REST/SOAP → SFTP/CSV. Normalize all of it into a single domain model so downstream rules don’t care which pipe delivered the data.
Middleware vs Direct
- Use middleware when you need routing, transforms/mapping, central monitoring, or to hedge vendor churn—classic healthcare app integration needs.
- Go direct for low-latency paths (e.g., slot holds in appointment scheduling) or when a vendor’s API is stable and well-scoped.
- Hybrid works: shadow-write via middleware while reads come direct; flip once error budgets hold.
Rollout Pattern That Avoids “Big Bang” Regret
- Shadow writes for 2 weeks (read-only in downstream systems).
- Feature-flagged partial cutover by cohort/location.
- Auto-rollback if SLIs breach the error budget.
Specode’s Posture: Why This Ships Faster, Safer
Specode assembles intake as healthcare automation: an event-driven intake component pre-wired to scheduling, EHR integration, checkout, and the patient portal. Opinionated defaults—idempotency, audited change history, PII-safe logging, and backoff/retry—deliver resilient flows and real-time updates without racking up integration debt.
Compliance Gotchas That Surface in Audits
Skip the HIPAA compliance basics—auditors assume you know encryption and BAAs. What catches teams during electronic patient intake audits are the workflow gaps nobody tested under scrutiny.
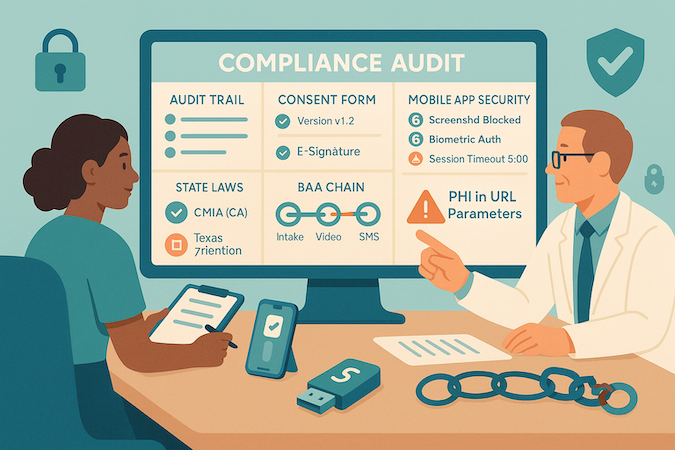
Audit Trail Incompleteness as the Top Flag
California's CMIA requires automatic recording of who changed what and when in electronic records—if your patient check-in app lets staff edit insurance info without logging identity, date, and reason, you're exposed. Most custom builds forget this until an auditor asks "who updated this Medicaid ID on June 3rd?"
Consent Form Versioning Failures Wreck Compliance Audits
You can't prove which version of a consent form a patient signed if your system overwrites forms or lacks immutable timestamps. E-signature compliance demands date/time stamps, IP logging, and demonstrated intent—checkboxes and electronic signatures alone don't cut it.
Mobile App Security Gets Scrutinized Hard
- screenshot prevention for PHI screens
- biometric auth options
- aggressive session timeouts
PHI leaking into URL parameters or browser LocalStorage (common in rushed custom builds) is an instant finding.
State-Specific Layers Do Matter
California CMIA extends beyond HIPAA, covering mental health apps and requiring stricter breach notice. Texas mandates 7-year retention from last treatment (longer for minors)—delete records early and you're liable even after closing your practice.
The "we'll add it later" trap is expensive: retrofitting audit logs, consent versioning, and change tracking into production code costs 5x more than building it in from day one.
BAA Daisy-Chains Create Audit Nightmares
Your intake vendor touches PHI, your video vendor touches PHI, your SMS vendor touches PHI—each link needs a signed BAA and documented controls. One weak link and the entire chain collapses under audit pressure.
ROI Reality: Where Intake Wins and Loses Money
Vendors sell feelings; finance buys formulas. The working formula is:
ROI = (Throughput Uplift + Utilization Uplift + Leakage Recovery + Attach Revenue) − (One-time + OpEx + Adoption Drag).
Revenue Levers
- Throughput uplift (minutes saved). Net 3–7 min/patient (post-exceptions) × weekly volume → extra visit capacity. Tie it to wait time reduction and your contribution margin, not list price.
- Utilization uplift (no-shows ↓). If reminders move no-shows 20–50% (studies: up to 38%), that’s kept visits × margin—period.
- Leakage recovery (data accuracy). Pre-visit insurance verification and cleaner demographics prevent denials; with 78% of providers struggling to collect >$1k in 30 days, even 2–3% recovery is meaningful to the revenue cycle.
- Attach revenue. Intake surfaces services (DX screens, labs, memberships). Model as attach rate × avg attach contribution.
- Payment capture. Faster payment processing (co-pays, cards-on-file) turns intake clicks into cash sooner.
Cost Levers
- One-time: configuration, data migration, patient registration content, and training burn (hours × loaded hourly cost).
- OpEx: patient tech support, release testing, integration maintenance (version/API drift).
- Adoption drag: discount factor on all gains (e.g., completion × write-back success). Poor rollout can halve ROI regardless of tool.
Break-even + Sensitivity
- Break-even (weeks) = (One-time) ÷ (weekly_throughput_Δ$ + weekly_utilization_Δ$ + weekly_leakage_Δ$ + weekly_attach_Δ$ − weekly_OpEx)
- Sensitivity (quick checks):
Completion factor → ROI multiplier: 0.50 / 0.65 / 0.80
No-show delta (pp) → added kept visits/wk: 0 / +10 / +20 (for 200/wk volume)
Worked Example
Example: 200 patients/week. Adjust the inputs to your practice.
Assume 5 net minutes saved/patient, 20-min avg visit, $70 contribution margin/visit, no-show 18% → 12%, leakage recovery 2%, OpEx $1.5k/mo, one-time $15k.
- Throughput: (200×5)/20 = 50 extra visit-minutes → 2.5 visits × $70 = $175/wk.
- Utilization: 200×(0.18−0.12)=12 kept visits × $70 = $840/wk.
- Leakage: 200×0.02×$70 = $280/wk.
- Gross/wk: $1,295; Net/wk after OpEx (~$375) ≈ $920 → Break-even ≈ 16 weeks.
One Line for Execs
If the spreadsheet fails with adoption discounts applied, production will too. The same math applies in telemedicine app development—just change the margins and visit mix. Build your case like this, then decide the tooling. That’s how you justify a medical intake app.
Implementation Playbook: First 90 Days
Most teams treat intake rollout like flipping a switch. Ship the whole thing, hope for adoption, wonder why staff revolt. The teams that actually succeed treat it like a clinical trial: small cohort, tight feedback loops, iterative fixes.

Weeks 1-2: Workflow Mapping (Not Theory)
Shadow your front desk for two full days. Document every touch point—phone calls, paper forms, insurance card photos, the Post-it notes stuck to monitors. Those workarounds exist because your current system has gaps; your patient registration app needs to plug them, not create new ones.
Map patient types and their form variations. New patient vs returning. Cash pay vs insurance. Telehealth vs in-office. A one-size intake kills completion rates before you start.
Weeks 3-4: Form Design and Pilot
Pick 1-2 visit types—your highest volume, least complex scenarios. Build those forms mobile-first and test with real patients, not your IT team. Conditional logic sounds great until a 70-year-old hits a loop they can't escape.
Run the forms on actual phones in your waiting room. Watch where people get stuck. Resolve obvious blockers the same day when feasible.
Weeks 5-6: Staff Training and Parallel Runs
Train staff, then run paper and digital simultaneously for two weeks. Yes, it's double work. It's also your safety net when the system hiccups or a patient refuses to use a phone.
Daily 15-minute standups. What broke today? What's confusing patients? What's slowing staff down? Adjust forms and workflows in real time—don't wait for "phase two."
Weeks 7-8: Patient Communication Campaign
Multi-channel blitz: email, SMS, IVR, in-office signage. But skip the "we're going paperless office!" corporate speak. Tell patients why: faster check-ins, shorter wait times, pre-filled forms on their phone before they leave home.
Critical: avoid forcing 100% digital adoption. Have a paper backup for resistant patients. Forcing digital on a 15% holdout group tanks your staff notifications workflow and creates resentment.
Weeks 9-12: Monitor, Iterate, Optimize
Track completion rates by patient segment. Are seniors abandoning at insurance questions? Is queue management stalling because forms don't sync fast enough? Are staff still using self-service kiosk workarounds because the patient onboarding app misses edge cases?
Fix abandonment points weekly, not quarterly. The longer bad patterns persist, the harder they are to kill.
The gradual rollout mistake: Stretching this to six months kills momentum. Staff lose confidence, patients get mixed messages, and leadership questions ROI before you hit meaningful volume. Ninety days is aggressive but realistic—anything longer and you're just delaying failure or success.
When Intake Becomes Strategic Differentiation
Patient intake management app choices become strategic only when intake creates defensibility—not just convenience.
Test 1 — Moat Score
Does ≥40% of your differentiation or revenue path rely on intake logic (eligibility gates, routing, prior-auth triggers)? If yes, intake is product-core.
Test 2 — Data Gravity
Does intake generate net-new structured data that downstream systems actually use? Aim for ≥50% reuse across EHR, billing, and care pathways—think richer patient demographics plus clinically relevant patient data collection that drives rules, not just storage.
Test 3 — Orchestration Complexity
Happy path touches ≥3 systems (EHR, scheduling, payments/pharmacy) and ≥5 event types (Submitted, Amended, Signed, SlotHeld, PaymentAuthorized) with tight SLAs. You need event contracts, retries, and auditability—i.e., architecture, not a form plugin.
Decision Rule
- 0–1 tests true → buy (commodity intake; optimize rollout).
- 2–3 tests true → assemble/customize; own the logic and events while reusing HIPAA-ready primitives.
Smell Checks for the “Dangerous Middle”
If you’re scripting heavy vendor workarounds, mirroring intake data in a shadow DB, or bending scheduling to fit branching rules, you’ve crossed into custom territory—make it intentional, not accidental.
How Specode Helps Build Patient Intake Systems
Stop rebuilding plumbing. Ship workflows.
Start from a Working Baseline
- Branching questionnaires, e-signatures, audit trails, PHI-safe storage, mobile-first.
- You begin with a HIPAA-compliant intake flow, not a blank IDE.
Already Wired to Your Stack
- Scheduling auto-populates appointments from intake.
- Basic EMR pre-fills charts; checkout pulls demographics.
- Patient profile acts as single source of truth—no duplicate entry, no manual reconciliation.
Customize at the Right Layer
Build by chat—the AI changes fields, branching, and validation from plain-English prompts with an instant preview.
- Connect your own data early so the assistant shapes real screens and flows;
- Theme it end-to-end to match your brand.
When you need something bespoke, drop into code—or tap our Custom tier for managed help. No AI magic—sequence and ruthless focus.
Proof in Practice
- AlgoRX combined intake + eligibility screening + provider automation to create a Shopify-style medication checkout.
- Patients complete product-specific questionnaires; the system captures correct insurance information and clinical context up front, auto-routes to providers, and moves straight to fulfillment.
- Result: $1M+ in sales by month two—because the intake flow eliminated back-and-forth.
Speed + Control
- Pilot in days, not quarters.
- You own the code—extend intake rules or integrate services without gatekeepers.
Build the 20% that differentiates (care model, specialty-specific questions, provider-matching). Reuse the 80% that’s table stakes (secure forms, consent workflows, PHI handling, immutable logs). If you need a healthcare intake app that starts strong and stays flexible, this is the shortest path.
Start free on Specode—make one small change (“add consent + insurance eligibility on submit”), see it live, connect your sandbox EHR for write-back, then stack two weeks of wins and retire double entry for good.
Frequently asked questions
Use the 3-test diagnostic: moat dependence, data reuse downstream, and orchestration complexity. If two or more are true, treat intake as product-core and assemble/customize.
Aim for 70%+ with multi-step sequencing, pre-population, and short rescue nudges. Track by segment and fix the highest-drop step first.
Yes. Without write-back you create double entry, staff resentment, and silent abandonment. Adoption collapses even if the UX is great.
Start with one or two high-volume visit types, ship progressive intake, run paper+digital in parallel for two weeks, and measure minutes saved, kept-visit %, and denial rate weekly.
Offer an assisted or paper path and route exceptions to a short queue. Forcing 100% digital increases friction and undercuts staff buy-in.
Identity matching, eligibility loops, vendor rate limits, and slow UAT. Plan for retries, dead-letter queues, observability, and a shadow-write cutover.
Sequencing. Ask only what’s needed now, push sensitive fields later, and use conditional logic so patients never see irrelevant questions.
Implement immutable audit trails, consent versioning with timestamps, proper e-signature evidence, PHI-safe logging, and signed BAAs for every downstream vendor.
If intake is commodity, a basic tool is fine. If intake drives routing, eligibility, payments, or provider automation, Specode’s pre-wired components plus code ownership let you move fast without accruing integration debt.








