How to Build a Remote Physical Therapy Platform — Clinician-Approved, Payer-Ready
Want to create a physical therapy app that clinicians actually use and payers reimburse? Start by ditching the “Zoom with exercises” mindset. PT lives in numbers: goniometry-grade ROM, gait timing, balance metrics, and adherence trends tied to validated outcomes—not vibes.
Build for measurement, not meetings, then route that data into RTM-ready workflows, PT-specific EMR semantics, and a home-exercise-program engine that adapts without manual micromanagement.
This guide maps the stack that scales: camera+IMU hybrids for movement tracking, progression logic that beats reminder spam, RTM documentation that survives audits, and integrations that don’t double-chart. Ship it right and you get fewer denials, cleaner notes, and sessions that coach in real time—not a pretty portal that collapses at 500 concurrent users. 
Key Takeaways
- Measurement beats meetings: design a hybrid stack (camera + IMU) with a ≤150 ms coaching budget, use MediaPipe for most ROM, add IMUs for timing/occlusion, and push inference to the edge—accuracy by specialty, not by hype.
- HEP adherence is a closed loop: structured exercise library + adaptive progression tied to PROMIS/LEFS/DASH, passive wearable signals, and dashboards that escalate only outliers—no reminder spam, just measurable behavior change.
- Monetize the care loop or don’t ship: wire RTM correctly (98980 ≈ $50; 98981 ≈ $39, monthly time rules, interactive comm), keep EMR integration shallow where it saves time and native where it protects data semantics, and architect HIPAA-grade video/storage from day one. A clinic with ~50 RTM patients can add ~$53k/year—if the platform is built this way.
Why Generic Telehealth Fails at Physical Therapy
Most telehealth tools were built for primary care video consultations—quick check-ins, refills, maybe a rash photo. PT needs quantified ROM, gait, balance, and adherence trends you can defend to payers, not just a camera and a chat box.

Where Generic Telehealth Breaks
- No native RTM time capture or documentation for 98980/98981/99457/99458; interaction logs, data-review timestamps, and treatment updates aren’t structured for audits.
- HEP engines lack progression logic; patient engagement stalls beyond reminders; wearables aren’t integrated for passive tracking.
- Movement analysis arrives late; measurement accuracy and reliability stay unvalidated.
- Insurance verification and eligibility checks aren’t wired into scheduling, so hybrid care economics don’t pencil out.
- Shallow telehealth integration assumes a 15-minute visit model vs multi-week rehab cycles.
- EMR fields don’t map to PT outcome measures, multiplying documentation burden.
The Financial Pressure Cooker
Medicare pays about ~$50 for 98980 and ~$39 for each additional 20 minutes under 98981—but only with airtight time tracking and interactive documentation.
PT telehealth codes remain provisional through December 2025; the 2025 conversion factor fell another 2.83% to $32.35, and the therapy threshold rose to $2,410. Without RTM revenue and compliant workflows, margins compress fast.
What the Numbers Look Like in Practice
A clinic with 50 RTM-eligible patients can clear roughly ~$53,000/year from treatment-management codes—if the platform actually supports:
- time tracking
- auto-adjusting HEPs
- wearable data
- audit-ready trails
Teams that try to build a remote physical therapy platform atop generic stacks typically discover the missing pieces around month six—when denials hit and the “Zoom wrapper” reality sets in.
How Serious PT Teams Approach It
They avoid $300k+ retrofits by starting with components purpose-built for therapy: scheduling tied to RTM tracking, PT-specific EMR fields aligned to outcome measures, and telehealth integration that treats rehab as a longitudinal program.
If your stack can’t support a 12-week post-op plan with measurable progress and clean claims, you’re not shipping virtual PT software—you’re shipping risk. In other words, unless the platform is designed for therapy-grade measurement and reimbursement from day one, it isn’t an online physical therapy platform.
Movement Tracking Architecture
Telehealth physical therapy platform architecture: choose pose estimation and IMU placement that deliver goniometry-grade ROM and gait events within a ≤150 ms feedback budget—so clinicians get numbers they can act on, not another video feed.

Computer Vision for ROM: MediaPipe vs OpenPose
MediaPipe and OpenPose both do pose estimation, but they optimize for different realities:
- MediaPipe (mobile/edge, 33 landmarks): reliable for pose estimation at the bedside or living room. In practice, it keeps range of motion error tolerances in a clinically acceptable band for large-joint tasks (shoulder flexion, knee extension) and delivers smooth real-time feedback at 30 FPS on commodity phones (and far higher on modern iOS). If your goal is AI movement detection and adherence coaching, this hits the ROI sweet spot.
- OpenPose (research/lab, 18–135 keypoints): higher spatial fidelity and multi-person tracking, but it’s compute-hungry, pushing up latency and infrastructure costs. Useful for 3D motion capture–adjacent experiments and in-clinic assessments where you control the hardware.
Opinionated call: Use MediaPipe for most telehealth rehabilitation ROM workflows. Reserve OpenPose for controlled studies or group sessions where precision and multi-person tracking pay off.
When IMUs Beat Cameras
Cameras struggle with occluded limbs and out-of-plane motion. IMUs (ankle/foot/waist) win here:
- Gait events: heel strike/toe-off timing and stance/swing detection stay accurate across lighting, clothing, and angles.
- Balance work: subtle sway and weight-shift during Romberg/tandem stance are better captured via accelerometer/gyroscope than a front-facing camera.
- Real life > test room: patients wear wearable devices all day, so data is ecologically valid—no “performing for the camera.”
Rule of thumb: If precision depends on timing or the movement happens perpendicular to a lens (or off-camera), strap on at least one IMU.
Hybrid Approaches
The best movement tracking stacks are sensor integration first, not camera-only or sensor-only:
- Upper-body ROM & coaching: camera (MediaPipe) + on-screen cues for real-time feedback.
- Lower-extremity & 3D tasks: single foot-mounted IMU + camera to reduce joint-angle error and stabilize timing.
- Cost control: start with “one IMU + phone” rather than full-body wearables; expand only if outcomes demand it.
Integration notes
- Fuse streams early (timestamp alignment) and store synchronized snippets for audit/review.
- Run lightweight QC at the edge (phone) and heavier motion analysis in the cloud when bandwidth allows.
- Keep a clinician override in the UI; machines score, humans sign off.
Real Accuracy Targets by Specialty
Different PT domains have different error budgets. In orthopedic PT, stay within ±5° for joints and tighter for small ones; use MediaPipe for movements >90°, adding IMU validation for <40° arcs or end-range checks.
Neurological rehab prioritizes asymmetry, cadence, path deviation, and temporal gait metrics; go IMU-first for timing fidelity, with camera context. Vestibular PT demands head-motion precision (VOR), sway metrics, and perturbation timing; combine camera-based head tracking with IMU targeting sub-degree head angles and millisecond-level timing.
Engineering Checklist
- Latency budget: ≤150 ms for on-screen coaching; fail fast on low light/bad framing.
- Calibration: quick, patient-proof routines (anthropometrics, limb length) cached per device.
- Environment robustness: handle small rooms, variable lighting, furniture occlusion.
- Data model: store raw landmarks + derived metrics; keep versioned model IDs for auditability.
- Privacy: process on-device where possible; encrypt and segment PHI in transit and at rest.
Design hybrid by default and validate to spec; that’s how you ship a credible remote rehabilitation platform.
The HEP (Home Exercise Program) Adherence Engine
In virtual physical therapy app development, the adherence engine is the operational core: it must reduce clinician effort while increasing patient certainty—what to do today, whether it’s done correctly, and what happens next—in a physical therapy app that clinicians trust.

Smart Exercise Prescription (Not Static PDFs)
Ditch PDFs for a structured exercise library with multi-angle exercise videos and rich tags (region, difficulty, equipment, contraindications). Seed treatment plans from diagnosis-aware templates, then personalize with goals, baselines, and flags.
Encode exercise prescription rules so plans progress or regress automatically based on completion quality and pain feedback, while preserving clinician control and auditability. The result is a home exercise program that adapts in clear, explainable steps—driving patient compliance without manual micromanagement.
Adherence Tracking That Goes Beyond Reminders
- One-tap completion with optional pain/difficulty; anything >5 seconds kills follow-through.
- Passive activity signals to validate real effort and counter inflated self-reports.
- Dashboards that surface only outliers (missed streaks, rising pain, sub-60% completion).
- Contextual nudges tied to behavior patterns, not a fixed notification schedule.
Auto-Adjusting Difficulty Based on Real Outcomes
Tracking without adaptation is theater. Tie daily completions and pain signals to standardized measures (PROMIS, LEFS, DASH) and adjust the plan accordingly. If a patient overshoots targets or marks “too easy,” queue harder progressions for clinician approval; if adherence dips or symptoms flare, suggest modifications before disengagement.
The system proposes; the clinician disposes—every change logged with rationale to keep documentation defensible and the care loop tight.
Wearable Integration for Passive Monitoring
- Pull steps, active minutes, and sleep to validate effort without extra taps.
- Use light HR/HRV trends to explain fatigue-driven adherence dips and timing of progressions.
- Store device metrics alongside exercise events for longitudinal, audit-ready evidence of response.
Gamification That Doesn’t Insult Professional Athletes
- For newcomers: trajectory views and milestone notes (“20 sessions; knee flexion up 30%”) beat confetti.
- For competitors: comparative analytics vs baseline/contralateral limb (“quad 85% of uninjured; +25% in 3 weeks”)—data, not cartoons.
Build the adherence engine as a closed loop—prescribe, measure, adapt, and escalate only what needs attention—and your home exercise program becomes the reason remote rehab works, not a PDF attachment collecting dust.
RTM and PT-Specific Billing Architecture
When you create a physical therapy app, the billing layer determines whether you have a demo or a business. Most platforms nail the patient-facing UX but stumble on reimbursement architecture—and that gap costs practices real money every month.
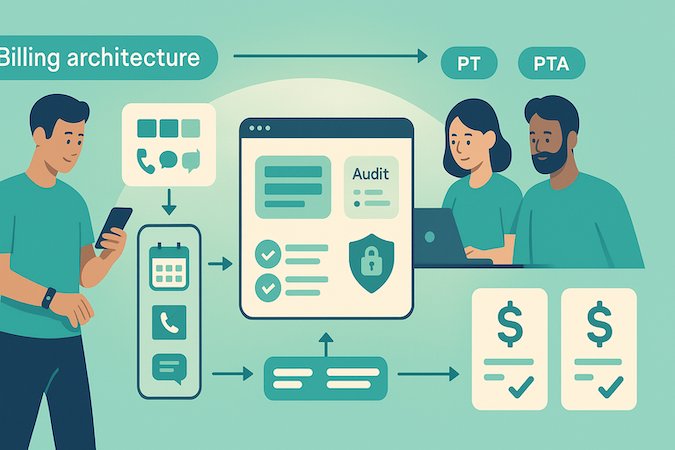
RTM codes opened a $50-per-patient revenue stream for PT in 2022, yet most platforms still don't support them properly. Here's what actually gets billed:
RTM Treatment Management (The Revenue Codes)
- 98980 – First 20 minutes of treatment management per calendar month (~$50.14 national average in 2025)
- 98981 – Each additional 20 minutes (~$39.14)
These codes reimburse PTs for time spent reviewing remote monitoring data, adjusting treatment plans, and interactive communication with patients—work that's always happened but never got paid until now.
What Trips Up Most Builds
The compliance requirements are surgical, and generic digital physical therapy solution frameworks miss them entirely:
Time Tracking Precision
You're tracking cumulative minutes per calendar month, not rolling 30-day periods. Most platforms default to 30-day logic because that's what RPM uses—instant audit failure. Your system needs to reset monthly, aggregate time across multiple patient interactions, and prevent billing unless you hit full 20-minute increments.
Interactive Communication Mandates
Medicare requires at least one interactive communication per month to bill 98980/98981:
- call
- video
- message requiring clinical judgment
Passive data review doesn't count. Your telemedicine app development needs to timestamp and categorize every patient interaction, distinguish clinical communication from admin messages, and auto-flag months where billing threshold is met.
Documentation Tripwires
For every RTM claim, you must document: device data reviewed, date/time of patient interaction, and clinical decisions that changed the treatment plan. Missing any element = denied claim. Build automated documentation templates that capture this data in the workflow, not as an afterthought.
Supervision Complexity
PTAs can contribute to monitoring time, but only under direct supervision when billed "incident to." Your system needs RBAC that tracks who reviewed what, ensures supervisory sign-off, and prevents billing for unsupervised assistant time.
Outcome-Based Contracts
Beyond Medicare, employers and ACOs want outcome measurement tied to cost. Smart platforms embed PRO-CTCAE scores, fall risk assessments, and functional outcome tracking directly into the RTM workflow—turning remote monitoring into proof of value for contract negotiations.
The billing integration isn't a feature; it's the foundation. Build it wrong and you're maintaining a very expensive patient engagement tool that doesn't generate revenue.
PT-Specific EMR Integration Challenges
Most PT EMRs were built around in-clinic, synchronous workflows. You can “integrate” with WebPT or Raintree, but what flows through the pipe often shreds clinical context or doubles clinician work.
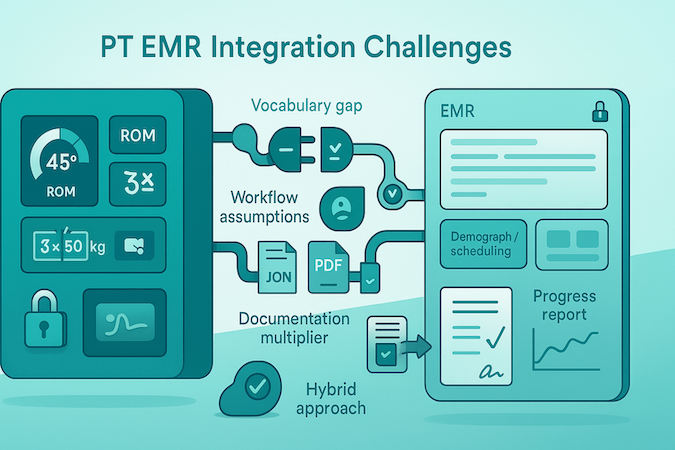
The Vocabulary Gap
- FHIR can store ROM and exercises in Observation/Procedure, but it wasn’t designed for joint-angle granularity, reps, resistance, or functional patterns—context gets flattened into text.
- PT semantics (e.g., phase-based prescriptions, targeted muscle activation, interval counts) exceed what common profiles expect, so precision data becomes unqueryable later.
- Result: your patient progress tracking loses computability; clinicians see words, not structured metrics they can trend.
Workflow Assumptions That Break
PT EMRs assume therapist-present sessions with immediate documentation. Remote rehab flips that: patients record at home, devices capture movement asynchronously, and therapists review in batches hours or days later.
Where do provisional ROM values live before validation?
How do you represent adherence and symptom trends that don’t map to a scheduled encounter?
Most APIs weren’t designed for async review queues, provisional findings, or delayed attestation, so you end up bolting on side ledgers and reconciliation jobs.
The Data Model Maze
- One EMR models ROM as discrete fields per joint/plane; another tucks it into SOAP text; a third hides it in templates—same concept, three incompatible shapes.
- Exercise prescriptions may be library items with metadata, PDF attachments, or free text; rendering them uniformly in patient portal development requires custom parsers per EMR.
- Some systems store derived metrics only in narrative notes, so you can’t safely round-trip updates without losing meaning.
- Faced with this, teams duplicate data in their own store, defeating the point of “integration.”
The Documentation Multiplier
Therapists document once in your platform (video notes, movement analyses, progress reports), then again in the EMR for billing/compliance because notes endpoints are locked down or read-only.
Limited bidirectional write and rigid workflows imply there’s stalled automation and creeping double-charting overhead.
The Reality
Successful teams go hybrid: keep EMR connections shallow for demographics/scheduling; build native clinical workflows (exercise prescription, async review, scoring) where you control structure; export a concise, sign-ready progress report back to the EMR.
Make the platform clinically self-sufficient so integration becomes an enhancement, not a dependency, while preserving clean audit trails for patient progress tracking. That’s the pragmatic path for remote PT platform development.
Clinical Credibility Features That Make or Break Adoption
To build a telerehabilitation platform clinicians actually trust, design for clinical truth first and product polish second. The bar isn’t “more data”; it’s defensible measures, clear supervision, and physician-ready communication—the things digital therapy platforms too often bolt on late.
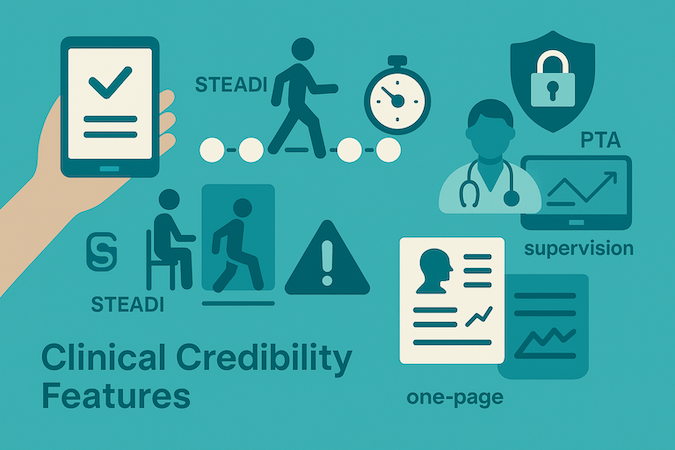
Validated Outcomes, Embedded (Not Bolted On)
Use validated instruments inline with care, not as extra forms. Auto-trigger outcome measures at intake and key milestones, pre-populate from existing data, and render results with functional interpretations clinicians and patients understand (“manages stairs independently,” not just a T-score). Keep scoring explainable, auditable, and tied to the plan of care.
Fall-Risk Automation That Respects Clinical Protocols
STEADI is a workflow, not a button.
- Provide guided setup wizards (10-foot path marking, camera placement cues).
- Capture and timestamp events for Timed Up and Go and 30-Second Chair Stand.
- Structure 4-Stage Balance prompts to reduce user error.
Build safety interrupts that flag unsafe movement patterns in real time and route the session to a clinician—under strict HIPAA compliance (encrypted media, audit-logged alerts, least-privilege access).
DPT–PTA Supervision Without Friction
General supervision only works if oversight is visible. Give PTs live views of PTA caseloads, one-click escalation on complex cases, and automatic supervision logs that include who reviewed what, when, and why.
Track conference requirements and time-based rules so the platform prompts the right documentation before billing trips a compliance wire.
Physician-Readable Summaries That Change Referrals
Turn outcomes into decisions, not spreadsheets. Combine functional milestones with pain assessment signals so referring physicians see causal progress (“pain interference down as step-ups increased,” “return-to-stairs achieved”). Keep the summary to one page, link to supporting evidence, and preserve the trail:
- scores used
- thresholds crossed
- clinical rationale for changes.
Red-Flag Detection and Escalation You Can Defend
Detect patterns that warrant immediate attention—sudden balance deterioration, new neurological signs, atypical pain trajectories—and trigger encrypted, role-aware notifications. Every alert should carry context (trend lines, recent exercises, medications) and write its own audit record to support after-action review and quality improvement—again, HIPAA compliance by default.
Clinical credibility isn’t a feature set; it’s disciplined workflow design. Embed validated outcomes, operationalize fall-risk protocols, make supervision observable, translate results for physicians, and escalate red flags with evidence. Do that, and your section earns trust on day one—because it behaves like a clinic, not a camera app.
Technical Stack Decisions for Scale
Most PT teams waste months debating frameworks when the scale decisions live in infrastructure. The gap between “works in demo” and “supports hundreds of concurrent exercise sessions with corrective feedback” is about video handling, real-time ML, compliant storage, and edge architecture—not React vs Vue.

Video Infrastructure That Handles Movement Analysis
- Pair 20–30 fps RGB streams with event-based sensor data to capture compensations at low bandwidth and sub-frame latency.
- Pick codecs for the real world: H.264 trades a bit of processing for big bandwidth savings; MJPEG is CPU-light but bandwidth-hungry—choose based on home Wi-Fi vs clinic fiber.
- Use adaptive bitrate and jitter buffers; align to the global coaching budget (≤150 ms end-to-end) so mid-rep corrections actually land.
Real-Time ML at the Edge
Train centrally; infer on-device or at regional edge nodes. That keeps corrective cues instantaneous and resilient when connectivity dips. Cache pose sequences and interim assessments locally, then sync in the background so the therapist dashboard stays responsive and the patient portal remains useful even when the cloud blips.
This is where physical therapy software development earns trust: graceful offline behavior, deterministic model versions, and clear fallbacks when inputs are noisy. Tie event streams to audit trails, and make escalation pathways deterministic—no black boxes.
HIPAA-Compliant Storage for Video Assessments
- Enforce AES-256 at rest, TLS 1.2+ in transit, and BAAs with every vendor that touches PHI; immutable audit logs for view/export/delete.
- Separate compute from PHI: run pose estimation on anonymized frames, then attach derived metrics to patient IDs post-extraction (least-privilege by design).
- Decouple raw video from appointment scheduling and secure messaging services so operational features ship fast without expanding your compliance surface.
Edge Computing for Latency-Sensitive Features
For balance work and gait coaching, edge processing is the difference between catching a faulty rep and documenting it after the fact. Keep lightweight models at the edge for instant cues, reserve cloud for longitudinal analysis and outcomes, and fail gracefully to guidance-only modes when inputs are unreliable.
Engineer for reliability under real-world constraints—codec choices, edge inference, compliant storage, and offline tolerance—and you don’t just pass a demo; you build a teletherapy platform.
How Specode Helps Build PT-Specific Platforms
If the prior sections felt like a gauntlet of PT-specific landmines, you’re not wrong. Most teams hit walls at movement tracking, RTM documentation, or EMR gymnastics—then blow timelines solving problems we’ve already cracked.
Advantages (what you get on day one):
- HIPAA-first telehealth video that can ingest movement data from MediaPipe or IMUs; purpose-built for assessment, not generic conferencing.
- Secure, audit-ready storage for assessment videos (immutable logs; PHI-safe defaults).
- Flexible EMR components you can mold to PT workflows without rewriting chart logic.
- RTM-ready tracking: time logs and code-specific documentation without end-of-month note scraping.
- AI-assisted assembly to stand up auth, scheduling, secure video pipelines, messaging, and dashboards fast—while you still own the code. The AI builder will code anything you want and help you integrate it.
- Clear integration stance: out-of-the-box Canvas path or built-in basic EHR; others case-by-case via native APIs or middleware.
Allheartz—a computer vision PT platform doing real-time pose detection and goniometric analysis—shipped their MVP in six months. They focused engineering effort on their ML models and athlete-specific UX while we handled auth, scheduling, secure video pipelines, and EHR integration. Result: 50% fewer in-person visits, 80% less clerical work, and provable ROM measurement accuracy.
You don’t need quarters reinventing consent flows or audit trails when you could be iterating on exercise progression logic and outcome dashboards. Start with proven components (free), keep code ownership, and concentrate budget where you differentiate—that’s how teams develop a virtual PT platform clinicians adopt and payers reimburse.
Frequently asked questions
Aim for goniometry-grade ROM (≈±5° on major joints), use camera-based pose estimation for large arcs, and add IMUs for short arcs, timing-heavy gait, or occlusions. Keep end-to-end feedback under ~150 ms with edge inference so mid-rep cues land on time. Hybrid camera+IMU is the default, not the exception.
Replace PDFs with a structured exercise library and multi-angle videos, wire progression/regression to PROMIS/LEFS/DASH and daily pain/completion signals, and keep input friction to seconds. Use passive wearable data, and have the therapist dashboard surface only outliers—missed streaks, rising pain, sub-60% completion—so clinicians coach, not scroll.
Go hybrid. Keep EMR links shallow for demographics/scheduling, run native clinical workflows (exercise prescription, async review, scoring) in your platform, and export a concise, sign-ready progress report back to the EMR. That preserves PT-specific semantics, avoids double-charting, and keeps the patient portal consistent across EMRs.
Track cumulative minutes by calendar month (not rolling 30 days), capture at least one interactive communication (call/video/clinically-judged message), and auto-document device data reviewed, timestamps, and treatment-plan changes. Enforce RBAC/supervision so PTAs’ time is counted correctly. Tie all of it to audit-ready logs to survive reviews.
Use codecs matched to bandwidth (H.264 vs MJPEG), pair RGB with event-based data for low-latency analysis, infer at the edge with offline caching so the therapist dashboard and patient portal stay responsive, and treat PHI like plutonium: AES-256 at rest, TLS 1.2+ in transit, BAAs for every vendor, anonymized frames for compute, and immutable audit logs.








