A Guide to Integrating HIPAA-Ready Scheduling Components with Stripe Payments
Stripe tutorials work in e-commerce because “pay, then fulfill” is linear. In healthcare, the moment you collect payment changes clinical ops, compliance, and cash flow. Pick the wrong timing (pre-pay, post-visit, hybrid) and you’ll either depress conversions or deliver unpaid care.
On top, HIPAA requires a single audit chain that links the charge to the appointment and encounter—something Stripe’s logs don’t do for you. And when cards fail ten minutes before a visit, generic retry logic isn’t enough; you need failure handling that protects provider utilization and patient trust.
This guide shows how to wire Specode’s Scheduling, Checkout, Patient Profile, EMR, and Notifications so appointments, payments, and documentation stay in lockstep—with audit trails an auditor actually wants.
Key Takeaways
- Payment timing is your first architectural decision
Pre-pay reduces no-shows; post-visit aligns capture to documented CPTs; hybrid needs deposits plus reconciliation. Choose explicitly for your care model, or you’ll trade conversion for bad unit economics (or vice versa). - HIPAA demands a unified audit chain—Stripe alone won’t cut it
Auditors expect Patient ID → Appointment ID → Payment ID → Encounter/Outcome. Store this bridge in a HIPAA-compliant database and reference Stripe IDs as foreign keys; do not rely on Stripe metadata to carry PHI context. - Failure handling must preserve clinical workflow, not just “retry”
For T-10 declines: notify providers immediately, give patients a one-click retry, and release the slot on SLA; back this with idempotency keys, webhook ordering/dedupe, selective polling for time-critical states, and payout holds for post-visit models. Test every scenario with Stripe’s cards.
Why Scheduling + Payment Integration Is Harder in Healthcare
In e-commerce, payment happens before fulfillment. Simple. In healthcare, when you collect payment changes everything.

Payment Timing Affects Clinical Workflow
- Pay-before: Reduces no-shows but feels transactional for trust-driven services. Works for direct-to-consumer telehealth and wellness visits where patients expect upfront pricing.
- Pay-after: Matches traditional medical billing but opens you to payment capture failures after clinical services are delivered. Providers already spent 30 minutes with the patient—you can't "refund" their time.
- Hybrid (deposit + balance): Mirrors insurance co-pay models but requires reconciliation logic that connects insurance verification, encounter documentation, and balance calculations.
Choose wrong and you'll either hurt conversion (patients abandon at checkout) or tank unit economics (providers deliver unpaid care). There's no "best practice"—only trade-offs you need to map to your specific care delivery model.
HIPAA Audit Trails Must Connect Financial and Clinical Data
PCI-DSS handles payment security. HIPAA covers protected health information. The problem? Every payment in healthcare connects to an appointment, which connects to an encounter, which contains PHI.
You need an audit trail that answers: Who paid for what appointment, when was that appointment, what clinical service was delivered, and what was the outcome?
Stripe's logs capture payment events. Your EHR captures clinical events. But HIPAA auditors expect a unified trail that connects both—and most teams don't build it until they're scrambling before an audit. The logging isn't hard; remembering to log the right identifiers at the right moments is what catches teams off guard.
Last-Minute Payment Failures Tank Utilization
A declined card in e-commerce is a lost sale. A declined card 10 minutes before a scheduled telehealth visit is:
- A provider sitting idle during their booked slot (utilization loss)
- A patient who believes they have an appointment (trust erosion)
- A scramble to notify, retry, or release the slot to another patient
Generic payment retry logic doesn't account for appointment timing constraints. You need failure handling that understands clinical workflows: notify the provider immediately, give the patient a fast retry path, release the slot if payment can't be recovered in time.
If you're still figuring out your payment timing model, pause here. The architecture decisions in the next sections assume you already know when you're collecting payment. If you're unsure, talk to your finance lead or review how similar services in your vertical handle payments.
Specode's Scheduling Component: Built for Payment Integration
Most healthcare scheduling tools treat payments as an afterthought—maybe you’ll bolt on Stripe later, maybe you won’t. Specode’s scheduling component does the opposite: it’s architected from day one to handle the messy intersection of appointment booking, payment capture, and clinical workflow.
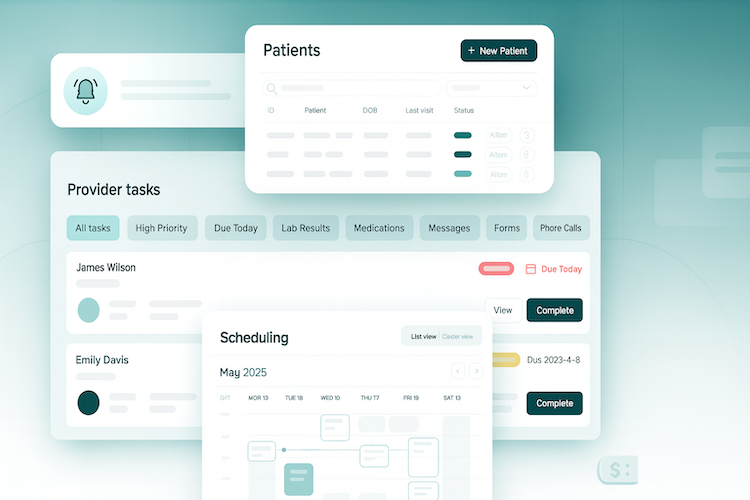
The core scheduling capabilities cover what you’d expect from any production-grade system:
- real-time availability syncing across providers
- patient-driven slot selection (by provider or first-available)
- specialty filters for faster discovery
- appointment types/durations and availability exceptions (vacations, holidays)
- automatic conflict detection
- configurable buffer times between appointments
These map to standard patient and provider workflows (24/7 online booking; provider schedule management) you’d expect in a clinical-grade module.
What sets it apart is that every booking event exposes clean payment hooks, so you’re not fighting the framework when it’s time to collect money.
Here’s where those hooks live: the scheduling component emits three key events—slot selected, booking confirmed, and booking canceled. Each event carries the appointment context (patient, provider, service type, timing) and connects to whichever payment pattern your business model requires.
You’re not reverse-engineering someone else’s opinionated flow; you’re wiring your logic into predefined extension points. Specode supports three payment timing patterns, and you pick the one that fits your model:
Deposit-to-Book
Means payment happens before the appointment confirms. The patient selects a slot, the Checkout component collects payment, and only after Stripe confirms does the booking lock in.
This pattern cuts no-shows dramatically because patients have skin in the game. Best for direct-to-consumer telehealth, wellness visits, and elective services where the provider’s time is the scarcest resource.
Post-Visit
This approach flips the sequence: patient books freely, the visit occurs, the provider completes documentation in the EHR component, and then payment captures based on the CPT codes logged.
This pattern fits provider marketplaces and insurance-based practices where billing depends on what actually happened clinically.
Hybrid
The hybrid pattern splits the difference: collect a deposit (estimated co-pay) at booking, deliver the service, reconcile with insurance, and either charge the balance or refund the overage. This matches how most insurance co-pay workflows actually operate in the real world.
Orchestrated, Not Isolated
The scheduling component hands off cleanly to Checkout (payment collection), Patient Profile (auto-populated billing info), and basic EHR (encounter creation that can trigger post-visit charges)—and is enhanced further with Telehealth (auto-generates secure video links per booking) and Provider Search (helps patients find and filter the right clinician before booking).
State synchronization across these components is baked in, so booking, payment, and encounter statuses stay aligned without custom glue code.
Pattern 1 - Deposit-to-Book Integration
This pattern works when you want payment before clinical services—direct-to-consumer telehealth, wellness coaching, elective consultations. Payment friction reduces no-shows by 40-60% in most implementations, and you avoid the "delivered care, can't collect" problem.
The Flow Is Clean
Patient selects slot → Specode's Checkout component collects card → Payment Intent confirms → Appointment books → Visit link generates. If payment fails, the slot stays open—no ghost bookings, no provider downtime.
HIPAA Logging Requirements
Every payment event must tie back to patient id + appointment id + payment id. Stripe's logs handle PCI-DSS; you own the PHI connection. Specode's audit trail captures this natively—who paid what, for which appointment, with what clinical outcome.
When Cards Decline
Show immediate retry with alternative payment options (Apple Pay, Google Pay). Release the slot after 10 minutes so it doesn't stay falsely blocked. Notify the patient via SMS/email with a 1-click return-to-checkout link.
Testing Before Launch
Use Stripe's test cards to simulate declines, 3D Secure flows, and successful payments. Validate that failed payments don't ghost-book slots and successful payments generate visit links within seconds.
Pattern 2 - Post-Visit Payment Integration
This pattern fits provider marketplaces, insurance-based practices, or anywhere billing complexity demands clinical documentation first. The key constraint: you can't calculate the final charge until after the provider completes their notes and assigns billing codes.
The flow: Patient books a slot (no charge yet) → visit happens → provider documents in the basic built-in EMR → CPT codes drive charge amount → Stripe captures payment.
Implementation Sequence
Configure Specode's scheduling component to create appointment confirmations, not payment charges. The booking is real, but Stripe stays quiet until documentation triggers it.
Wire the EMR billing module as your payment trigger. When a provider finalizes an encounter and assigns CPT codes, that event should fire a webhook to your payment logic. Map CPT codes to charge amounts in a lookup table.
For marketplace models, implement split payments here: platform fee to you, provider payout to them. Stripe Connect handles this cleanly, but you'll need to decide hold timing (immediate split vs delayed payout after services rendered).
Why documentation matters: CPT codes aren't arbitrary. They reflect complexity and time spent, which insurance and patients expect to match clinical notes. SOAP notes provide the clinical justification; billing codes translate that into dollars. Miss this link and you're defending charges without evidence during disputes.
HIPAA Audit Trail
Track the entire sequence: appointment id → encounter id → CPT code(s) → payment intent id → capture timestamp. Stripe logs the payment side; your HIPAA-compliant database connects it to the clinical encounter.
When Capture Fails
Provider already delivered care—you can't "undo" that. Build retry logic with patient notifications, and put provider payouts on hold until payment clears. If retries exhaust, escalate to collections or write-off workflows.
DyadSync’s approach: They implemented post-visit payments for anesthesiologist coverage, tying documentation completion to payout triggers—ensuring clinicians got paid reliably while maintaining clean audit trails between scheduling, service delivery, and financial settlement.
Pattern 3 - Hybrid Integration
The hardest payment pattern to get right: collecting just enough upfront to reduce no-shows while deferring final charges until you know what insurance actually paid.
When this pattern fits: Insurance co-pays where the full patient responsibility isn't clear until claims process. High-value services where you need skin in the game at booking but can't ethically charge the full amount before delivery. Estimated patient responsibility scenarios where the "estimate" matters more than the billing department wants to admit.
The Flow That Works
Patient completes Intake Forms (insurance details captured) → Specode's Basic EMR stores eligibility data → Patient selects slot → Checkout component collects deposit based on verified coverage → Payment method stored for later → Appointment confirmed → Visit occurs → Claims processed → Final balance calculated → Remaining charge or refund posted automatically.
Implementation Sequence
Wire Specode's scheduling component to trigger Checkout with a deposit amount (not full charge). The Intake Forms component has already gathered insurance details and verification—that data lives in the EMR before the patient ever hits scheduling.
Create Stripe PaymentIntent for deposit while saving the PaymentMethod ID to the patient's profile for later use. After the visit, your reconciliation logic compares insurance payment against total charges—if patient owes more, capture the balance using the stored payment method; if you overcharged, issue a partial refund through Stripe.
Why Intake Forms matter here: You're not flying blind on the deposit amount. Insurance verification already happened during patient onboarding, so your deposit calculation can reference real coverage data instead of guessing. This reduces awkward balance adjustments later.
HIPAA Reality Check
Your audit trail must connect the entire flow:
- intake forms
- deposit transaction
- appointment
- encounter
- final reconciliation
When you charge a balance three weeks after the visit, that charge needs traceable justification in clinical documentation. Refunds need the same—if insurance paid more than expected, the refund amount and reason go in the audit log.
Test these scenarios before launch: Overpayment requiring refund. Underpayment requiring additional capture. Insurance denial forcing full patient responsibility. Payment method expired between deposit and balance charge.
The HIPAA Audit Trail Most Teams Miss
Most teams wire up Stripe, see PCI-DSS compliance badges, and think they're done. They're not. PCI-DSS tracks payment security; HIPAA demands you trace why the payment happened and what clinical event it funded.

Stripe's logs show card charges—they don't connect those charges to appointment IDs, encounter records, or clinical outcomes. That gap is what sinks you in an audit.
Here's the chain HIPAA auditors expect: Patient ID → Appointment ID → Payment ID → Encounter ID → Clinical Outcome. Every refund, failed charge, or retry needs clinical context. If you refund a canceled appointment, your audit trail should show why it was canceled (patient no-show vs provider unavailable) and who authorized the refund. Without that, auditors assume you're leaking PHI or failing to secure financial ePHI properly.
What Auditors Review
- Can you reconstruct the payment-to-care sequence for any appointment?
- Are payment events (charge, refund, dispute) logged with clinical justification?
- Do your logs capture who accessed payment + PHI data and when?
Storage Matters
Don't store audit details in Stripe metadata alone—it's not designed for PHI retention rules. Use a HIPAA-compliant database for the clinical-payment bridge, and reference Stripe IDs as foreign keys. Specode's scheduling, checkout, and Basic EMR components maintain this audit trail by default: booking events sync with payment states, encounter documentation links to charges, and refunds carry clinical justification fields.
Building Failure Handling That Preserves Clinical Workflow
Payment failures in healthcare aren't just tech problems—they're clinical workflow bombs. A declined card 10 minutes before a visit leaves your provider idle, your patient confused, and your next appointment delayed. Unlike e-commerce where a failed payment just means a lost sale, healthcare failures cascade into scheduling chaos, wasted clinical time, and trust erosion.
The patterns we covered earlier (deposit-to-book, post-visit, hybrid) each have failure modes already addressed in their implementation flows. This section focuses on the technical architecture that makes those failure handlers actually work—because the difference between "we handle failures" and "our failure handling preserves clinical workflow" is in the details most teams skip.
Preventing Duplicate Charges During Retry Logic
When you're automatically retrying failed payments, idempotency isn't optional—it's how you avoid charging a patient three times for one visit. Stripe's Payment Intents handle much of this, but you need to implement idempotency keys throughout your retry logic.
Best practice: Generate a unique idempotency key combining appointment_id + payment_attempt_number + timestamp. Store this key with each payment attempt so your retry logic never creates duplicate charges. If a webhook fires twice (common with network instability), your system should recognize the duplicate event and ignore it rather than processing the payment twice.
Specode's Checkout component includes idempotency handling by default, but if you're adding custom payment logic on top, maintain the same pattern: one unique key per payment attempt, logged in your audit trail, checked before every charge.
Ensuring Stripe Events Trigger Correct State Changes
Stripe webhooks are your source of truth for payment state changes, but they're not 100% reliable. Network issues, server downtime, or misconfigured endpoints can cause webhook failures—leaving your scheduling component and payment records out of sync.
Verification approach: After creating a Payment Intent, poll Stripe's API every 30 seconds for up to 5 minutes to confirm the charge status. Don't rely solely on webhooks for time-critical state changes (like confirming a booking before a visit starts). Use webhooks for audit logging and eventual consistency, but poll the API for immediate decisions.
Webhook signature verification: Always verify Stripe's webhook signatures before processing events. Attackers can spoof webhook requests to trigger fraudulent refunds or mark unpaid appointments as complete. Specode's payment integration includes signature verification by default, but if you're customizing webhook handlers, don't skip this step.
Testing Payment Failures
Stripe provides test card numbers that simulate every failure mode you need to handle. Don't skip this testing—production payment failures are not the time to discover your retry logic has a bug.
Run through all payment patterns with test cards, verifying that your notifications fire correctly, audit logs capture every event, and provider/patient dashboards reflect accurate state. If you're building post-visit payment capture, test the scenario where a patient deletes their payment method between booking and visit completion—your capture logic needs to handle this gracefully.
Orchestrating Care and Cash Flow: How It All Connects
Think of Specode's components like a well-run clinical team—each member has a clear role, knows when to hand off, and the whole system runs smoothly without anyone micromanaging every interaction.
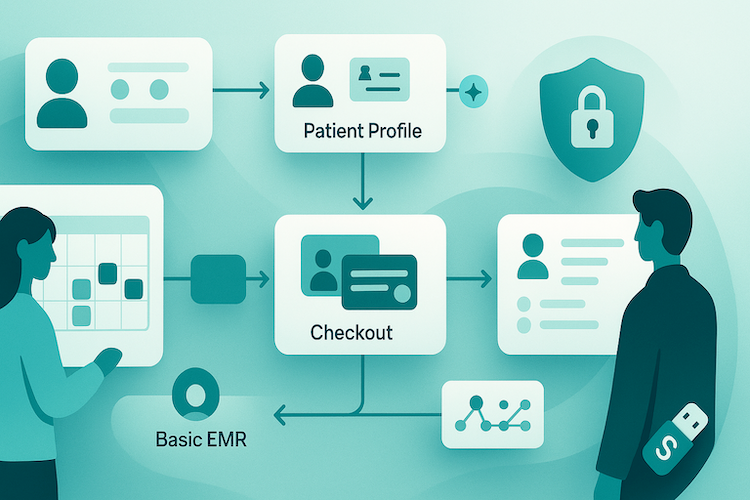
When a patient books and pays for a visit, here's what happens behind the scenes:
Patient picks a time slot
The Scheduling component shows available times based on your provider calendars, handles double-booking prevention, and reserves the selected slot for a few minutes while payment processes.
Payment gets collected
The Checkout component steps in automatically to collect payment details. It's already configured for HIPAA compliance and connects directly to your Stripe account. The patient enters their card information once, and it's securely stored for future visits.
Booking gets confirmed
Once payment clears, Scheduling converts that temporary hold into a confirmed appointment. The system now has three pieces of information connected: who the patient is, which appointment they booked, and which payment corresponds to it. That connection is your audit trail—the thing that proves you're tracking financial and clinical data properly.
Patient Profile fills in next time
The Patient Profile component quietly saves billing information during that first checkout. Next visit? Everything pre-fills. One less reason for patients to abandon booking halfway through.
Reminders go out automatically
The Notification component sends appointment confirmations immediately, then schedules reminder texts and emails for 24 hours and 1 hour before the visit. No manual calendar management, no forgotten follow-ups.
Clinical notes trigger final payments (for post-visit models)
If you're running a model where patients pay after the visit, your provider completes the visit note and billing codes in the Basic EMR component. When they mark it complete, that signals Checkout to charge the stored payment method. The appointment, the clinical documentation, and the payment all connect automatically.
Refunds and balance adjustments happen seamlessly
For practices using the deposit model (patient pays estimated co-pay up front, final balance calculated after insurance processes), the system handles the math. If the patient overpaid, it refunds the difference. If they underpaid, it charges the balance. No spreadsheets, no manual reconciliation.
Why This Setup Works for Busy Practices
Traditional custom-built systems force you to choose: either you get a rigid, one-size-fits-all solution that doesn't match your workflow, or you spend months (and significant budget) building from scratch.
Specode's component approach gives you both flexibility and speed. The components already know how to work together—scheduling talks to payments, payments talk to clinical records, everything logs to your HIPAA audit trail. But you're not locked into a specific sequence.
How Specode Helps Integrate HIPAA-Compliant Scheduling with Stripe Payments
If your goal is simple—let patients book, pay, and receive care without breaking clinical flow or audit readiness—Specode gives you the shortest path: composable, HIPAA-aware building blocks that already talk to Stripe and each other, so you configure timing (pre-pay, post-visit, hybrid) instead of stitching plumbing from scratch. You keep the code and the flexibility.

Composable, HIPAA-Ready by Default
Scheduling, Checkout, Patient Profile, Basic EMR, and Notifications are designed to hand off cleanly. Booking events expose payment hooks (slot-selected, booking-confirmed, booking-canceled), and your audit trail links Patient ID → Appointment ID → Payment ID → Encounter ID—what auditors actually expect.
Failure Handling That Protects Clinic Time
Idempotent retries, webhook ordering/dedup, and clear slot-release rules prevent ghost bookings and duplicate charges—especially when a card declines minutes before a visit. This is built to preserve provider utilization, not just “pass the charge.”
Speed Without Lock-in
Teams assemble HIPAA-ready apps dramatically faster (directionally, up to 10×), and a no-customization MVP can be stood up in ~a week. You still own the code and can extend or replace pieces anytime.
AI Builder
Describe your flow; the AI assistant scaffolds screens, data models, and wiring between components. Continue self-serve or drop to code at any point.
Proven Patterns, Not Experiments
Real teams have shipped these flows on Specode—so you’re configuring known-good patterns, not inventing them from zero:
- DyadSync (provider marketplace): streamlined scheduling plus post-visit capture tied to documentation; reliable clinician payouts and cleaner ops.
- AlgoRX (medication storefront): eligibility screening, multi-item cart, and integrated payments. Results: 15× ROI, $1M+ by month 2.
Pick your payment timing model, wire the components, and launch with audit-ready logs from day one—then customize what makes your practice different. That’s faster time-to-care, fewer ops fires, and code you truly control.
Start free on Specode—enable HIPAA-ready scheduling, paste your Stripe test keys, and add “collect copay at booking.” Preview in minutes, run a 10-appointment sandbox pilot, then flip to live when it clicks.
Frequently asked questions
Map payment timing to your care model: pre-pay for DTC telehealth/elective services to reduce no-shows, post-visit when charges depend on CPTs and documentation, and hybrid when deposits plus later reconciliation match insurance reality; optimize for either conversion or ops risk, but be explicit about the trade-offs.
Log the full chain—patient, appointment, payment, encounter, clinical outcome—and store it in your HIPAA-compliant database, referencing Stripe IDs as foreign keys; do not rely on Stripe metadata to retain PHI-linked audit context.
Notify the provider immediately, give the patient an instant retry with alternate methods, and release the slot on a defined SLA if recovery fails; ensure idempotent retries so you don’t double-charge or ghost-book.
Use idempotency keys scoped to appointment and attempt, verify webhook signatures, process events in order with dedupe, and poll Stripe selectively for time-critical states so scheduling doesn’t drift from payment truth.
Run through all three timing patterns with Stripe test cards, simulate declines and 3DS, test T-window edge cases, expired or removed payment methods, over/under-payments, insurance denials, refunds, and confirm notifications plus state transitions are accurate in patient/provider views.









