How to Build a Chronic Care Management App That Actually Generates Revenue
Most healthcare apps die not because they lack features, but because they fail at reimbursement. Nowhere is this more brutal than in chronic care management app development.
On paper, Medicare offers $60+ per patient, per month for care coordination. In practice, fewer than 3% of eligible practices actually run profitable CCM programs. Why? Because the math is unforgiving. Compliance eats margins, workflows collapse under documentation rules, and platforms built as “patient portals” rather than revenue engines burn cash instead of generating it.
The good news: with the right technical architecture, compliance stack, and feature focus, CCM apps can deliver both patient outcomes and sustainable revenue.
Key Takeaways
- Revenue starts with compliance, not features
The fastest path to failure is treating CCM like a wellness app. Profitability depends on billing-first architecture: audit trails, time tracking, and Medicare code logic built into the foundation . - Volume beats complexity every time
Elaborate care plans and feature creep drain staff hours without increasing reimbursement. Standardized templates, streamlined consent, and hybrid time tracking let one coordinator manage 300–400 patients instead of 150–200. - Build vs. Buy is no longer academic
With APCM widening reimbursable longitudinal care, skip ground-up custom. Use a HIPAA-ready healthcare AI builder (Specode) to assemble CCM rails—time tracking, audit logs, consent, scheduling/messaging, EHR/claims connectors—and ship in as little as 6–8 weeks with code you control.
The $60 Per Patient Reality Check
Let's talk about the elephant in the CCM waiting room: $60. That's what Medicare pays nationally for CPT 99490 in 2025 – your first 20 minutes of care management services per patient, per month. Sounds straightforward until you realize most practices lose money on every patient they enroll.
Here's why the math gets ugly fast. That $60 covers everything: clinical staff time, documentation, care plan creation, medication reconciliation, provider coordination, and the audit trail Medicare demands.
Factor in enrollment costs (getting consent takes 15-20 minutes), monthly outreach attempts (3 calls average to reach one patient), EHR integration headaches, and suddenly you're underwater before you've helped a single patient manage their chronic diseases.
As one family practitioner put it, CCM often “takes 20 minutes to simply do the work around the work.”
The profitability breakdown most vendors won't show you:
- Revenue per patient: $60 base
- Direct costs: $35-45 in staff time alone
- Hidden overhead: Data normalization, eligibility checks, patient churn management
- Actual margin: Often negative without hitting 300+ enrolled patients
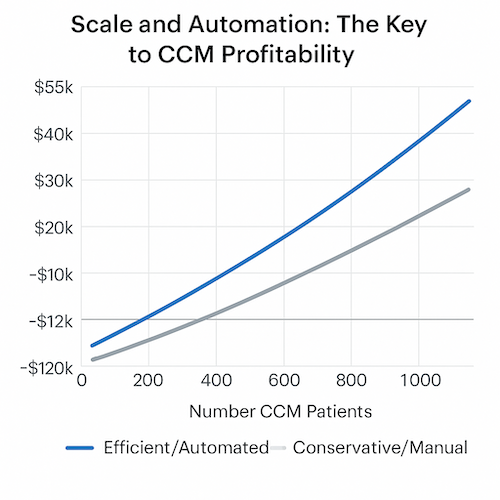
Why Scale and Automation Decide CCM Survival
This explains why less than 3% of eligible practices successfully run Medicare CCM programs. You need scale to survive – industry benchmarks suggest 1,000 patients minimum with two dedicated FTEs (full-time equivalent staff) to achieve that magical 40% profit margin everyone promises but few deliver.
The gap between a basic tracking app and a revenue-generating chronic care management app development platform? Automation and workflow intelligence. A tracking app logs blood pressure readings. A revenue platform automatically documents billable time, generates compliant care plans, triggers reimbursable touchpoints, and handles the Medicare audit requirements that keep you from clawbacks.
Quick Profitability Math for 2025
- Break-even point: 280-350 enrolled patients (assuming 70% monthly success rate)
- Staffing sweet spot: 1 FTE per 300-400 active patients
- Technology investment: $27-32 PMPM (per member per month) for platforms that actually handle billing workflows
- Time to positive ROI: 4-6 months with proper chronic care management application architecture
The brutal truth? Most CCM programs fail because they're built backwards – features first, revenue second. Successful programs start with billing requirements and work backwards to patient experience. That means your technical architecture must prioritize time tracking, audit trails, and documentation workflows over fancy dashboards nobody uses.
If you're not engineering for that $60 from day one – building automated time capture, streamlined consent workflows, and billing-ready documentation – you're building an expensive patient portal, not a CCM revenue engine.
Revenue Architecture: Build for Billing, Not Just Features
When you set out to build chronic care management app infrastructure, the temptation is to start with patient-facing features—medication reminders, care plans, secure messaging. But here's the reality: your technical architecture lives or dies by CPT codes 99490, 99439, and 99491. These aren't just billing codes; they're architectural blueprints that dictate how you structure data models, time tracking, staff permissions, and audit trails.

Medicare's reimbursement structure tells you exactly what to build. CPT 99490 requires at least 20 minutes of clinical staff time per month at approximately $60.49 nationally, while 99439 adds $45.93 for each additional 20-minute increment. Meanwhile, 99491 demands 30 minutes of direct physician involvement at $82.16. These aren't suggestions—they're the revenue foundation your app must support.
Why the 20-Minute Documentation Requirement Breaks Most Apps
That innocent-sounding 20-minute threshold for 99490 is where most CCM platforms fail their first audit. The problem isn't capturing 20 minutes—it's proving those minutes were legitimate, non-overlapping, Medicare-compliant activities. If clinical staff spends 30 minutes on an activity benefiting three CCM patients, you can only count 10 minutes toward each patient's service time.
Traditional EHRs treat time as an afterthought—a field you fill in after the fact. But CCM app development requires time to be a first-class citizen in your data model. Every interaction needs:
- Start and stop timestamps (not estimates)
- Activity categorization that maps to CMS-approved tasks
- Patient attribution for split-time scenarios
- Automatic exclusion of non-billable activities
Most developers discover this architecture requirement after building their MVP, leading to expensive rewrites when the first Medicare audit request arrives asking for granular time logs from six months ago.
The Hybrid Time Tracking Advantage
Pure automation sounds perfect: track every click, phone call, and message automatically. Pure manual entry seems simpler: let staff log their time like a timesheet. Both approaches fail in production.
Automated tracking captures everything but lacks context—was that 5-minute call about CCM care coordination or scheduling a routine appointment? Manual entry provides context but suffers from recall bias and missed entries. Many practices have implemented specialized software to track time and ensure all required components for CCM billing are met.
The winning architecture combines both:
- Automated capture of communication touchpoints (calls, messages, chart reviews)
- Smart prompting for activity classification during natural workflow breaks
- Batch review interfaces for end-of-day time validation
- Intelligent defaults based on interaction patterns (3-minute medication refill calls get auto-categorized)
Hybrid capture reduces missed entries and strengthens audit trails, where OIG reviews show documentation failures are common in CCM.
Single Provider vs Care Team: An Architectural Fork
Your choice between single provider and care team models isn't just organizational—it fundamentally changes your technical architecture. The single provider model (99491) requires tracking provider-specific time with forensic precision. The care team model (99490) needs sophisticated attribution logic for shared activities.
Care team architecture demands:
- Role-based access controls aligned with "incident to" billing rules
- Supervisor linkage for every clinical staff member
- Time aggregation across multiple team members
- Split-time calculation when activities benefit multiple patients
Single provider architecture requires:
- Provider-specific time buckets that exclude any delegated work
- Clear delineation between billable provider time and support staff activities
- Session management that prevents time overlap between codes
Most successful platforms support both models with configurable switches, but the underlying data models must be designed for this flexibility from day one.
The Post-G0511 Reality for FQHCs and RHCs
Starting July 1, 2025, G0511 will be decommissioned and FQHCs/RHCs must bill CCM services using standard CPT codes. This shift from a flat $74.20 rate to itemized billing creates both opportunity and complexity. FQHCs/RHCs can now bill 99439 for additional 20-minute increments, potentially offsetting revenue loss through volume.
Your architecture must now support:
- Granular time tracking to maximize 99439 add-on opportunities
- Workflow optimization to hit 40-60 minute monthly targets efficiently
- Parallel tracking of multiple care plans per patient
- Enhanced reporting to identify revenue optimization opportunities
The technical lesson is clear: billing codes aren't an afterthought in healthcare software—they're the foundation. Build for billing compliance first, then layer features on top of that revenue-ready infrastructure.
The Non-Negotiable Technical Stack for Medicare Compliance
Your audit trail architecture determines whether you keep the revenue you've earned. Medicare audits require detailed documentation of time spent delivering CCM services, including start and end times, type of service provided, and duration—and that's just the baseline.

CMS can revoke Medicare billing privileges for failure to respond to medical record requests, even for inadvertent failures like outdated contact information.
Why Your Audit Trail Architecture Matters More Than Your UI
HIPAA requires retention of audit logs recording access to and updating of PHI for a minimum of six years. But for CCM, you need
- immutable tracking of every interaction
- role-based access patterns proving appropriate supervision
- complete care plan versioning
The critical insight: Many CCM platforms are triggered just on time but not the scope of services being met. Your architecture must validate both duration AND activities performed. Missing this distinction is why platforms pass development but fail audits.
Before you ship a CCM MVP, run it through a healthcare app deployment checklist—it’s the fastest way to catch the “audit-fail” stuff (logging, access controls, environment hygiene) before Medicare makes you prove it retroactively.
Real-Time Documentation Requirements vs Batch Processing
Batch documentation at end-of-day is dead. Providers must document time spent delivering CCM services with start and end times recorded in the EHR as services happen, not reconstructed later.
This means synchronous patient data capture with immediate validation, event-driven streaming (think Kafka, not cron jobs), and instant scope-of-service gap detection. If staff logs 25 minutes but only documents medication reconciliation, your system flags the missing elements immediately—not during billing.
The Interoperability Mandate and What It Means for Your API Strategy
CMS requires Medicare Advantage organizations and Medicaid managed care plans to implement FHIR R4-based APIs with USCDI Version 1 and Version 3 data standards. This isn't just payer compliance—it fundamentally changes your chronic disease management app architecture.
By January 2027, your platform needs:
- FHIR-based APIs allowing third-party apps to access all claims/encounter data and clinical data
- Provider Access APIs sharing patient data with in-network providers including prior authorization information
- Prior Authorization APIs with 72-hour turnaround for urgent requests
Your EHR integration can't just pull data—it must expose standardized APIs for bidirectional exchange, map proprietary models to USCDI elements, and handle consent for multi-directional sharing.
State-Specific Variations That Break National CCM Platforms
State regulatory requirements are separate from Medicare requirements, creating compliance landmines. Texas HB300 requires breach notification for even single records. California CMIA adds marketing restrictions beyond HIPAA. New York SHIELD mandates specific technical safeguards.
Most critically, non-physicians must be legally authorized to provide CCM in the state where services are furnished. Your credentialing system needs state-specific scope-of-practice validation, not just NPI verification.
According to compliance toolkits and provider interviews, one of the most common audit failures is documentation that cannot prove full scope of services — e.g. care plans missing goals or medications — even when time is logged. Consent errors are a close second: missing elements like coinsurance disclosures or verification the patient isn’t receiving CCM elsewhere can trigger recoupments.
Building Tomorrow's Compliance Architecture
CMS continues pushing for additional standardized HL7 FHIR API access. Your architecture needs API versioning supporting multiple FHIR versions simultaneously, modular compliance engines for changing rules, and automated testing against evolving requirements.
The platforms that survive can prove every minute of care delivered, every consent obtained, and every data exchange completed. When you create chronic care management app infrastructure, remember: Medicare doesn't care about UX—they care about forensic-level documentation of compliance.
Essential Features That Actually Move the Revenue Needle
When you develop chronic care management app features, here's the uncomfortable truth: Medicare reimburses for comprehensive care coordination activities, while patients want simple medication reminders and appointment scheduling. The revenue-generating overlap? Surprisingly narrow.

Medicare pays for creating comprehensive care plans, documenting medication reconciliation, coordinating with multiple providers, and managing care transitions. Patients want to refill prescriptions with one tap, see their next appointment, and message their doctor. The platforms that succeed build for billing requirements first, then cleverly wrap patient value around those mandated activities.
The Care Plan Paradox: Why Complex Plans Reduce Revenue
Most developers assume elaborate care plans with detailed goals, interventions, and metrics would maximize reimbursement. The opposite is true. Complex plans take longer to create, require more updates, and reduce the number of patients staff can manage effectively.
The sweet spot for revenue generation:
- Template-driven plans that auto-populate from problem lists (5 minutes vs 20 minutes creation time)
- Three core elements per condition (goal, intervention, monitoring frequency)
- Quarterly batch updates instead of continuous tweaking
- One-click attestation for unchanged elements
A practice managing 400 CCM patients with simple, standardized plans generates more revenue than one managing 200 patients with detailed, personalized plans. The math is brutal but clear: volume beats complexity when you're working within fixed reimbursement rates.
Medication Adherence Tracking That Satisfies Auditors
In CCM, medication management is a billable, audit-sensitive core: Medicare expects documented medication reconciliation, interaction checks, and care-team follow-up on non-adherence. Stand-alone ‘adherence scores’ or pill-game UX don’t meet CCM requirements unless they translate into those documented clinical actions.
Build adherence features that document billable activities:
- Reconciliation workflows that capture discrepancies between prescribed and taken medications
- Provider alerts for non-adherence that trigger documentable outreach
- Pharmacy integration that auto-documents refill coordination (billable time)
- Timestamped interaction logs showing staff follow-up on adherence issues
Skip the patient-facing adherence apps—they don't generate billable encounters. Focus on tools that turn medication management into documented care coordination touchpoints.
Provider Communication Tools That Document Billable Time
Every provider interaction is potential revenue, but only if properly documented. Secure messaging alone doesn't cut it—you need communication tools that automatically capture billable elements while facilitating care coordination between healthcare providers.
The architecture that actually generates revenue combines auto-categorized message types (medication question = reconciliation time), duration tracking for async communications, provider-to-provider coordination logs, and batch documentation workflows for efficient time capture.
Your patient portal doesn't need every feature—it needs the ones that drive patient engagement in billable activities. Focus on consent management interfaces, care plan acknowledgment workflows, and structured symptom reporting that triggers billable nurse reviews. Everything else is expensive decoration.
Hidden Integration Challenges That Surface at Scale
You've mapped out your CCM workflow, nailed the time-tracking architecture, even sorted the CPT code logic. Then week 12 hits and your care coordinators are manually rekeying insurance eligibility because your EHR integration doesn't talk to the practice management system where the real billing data lives.
This is the integration tax nobody budgets for—the gap between what vendors promise and what actually breaks at 500 patients.
The Practice Management Blind Spot
EHRs handle clinical data beautifully, but resource constraints mean practices often split critical functions across multiple systems. Your EHR knows the patient has diabetes and hypertension, but it doesn't know their copay changed last month, their prior auth expired, or that they're scheduled for labs next Tuesday—that's all sitting in the PM system.
The painful reality: Most CCM platforms integrate with EHRs and stop there, missing:
- Real-time eligibility verification (determines if Medicare Advantage covers CCM)
- Authorization status for specialty referrals
- Appointment scheduling that drives your 20-minute monthly touchpoints
- Billing modifiers that determine whether you get $62 or $0 for that month's CCM services
This is why CCM platforms that only “integrate with the EHR” stall out at scale. If you need the PM/billing side to actually line up, see our guide to building a medical practice management app (and what to integrate first).
The Revenue Leak Nobody Talks About
Here's what happens when you skip billing system integration: Your CCM platform dutifully logs 47 minutes of care coordination for Mrs. Johnson. Your EHR documents her care plan updates. But the claim never makes it to your clearinghouse because nobody built the bridge between clinical documentation and revenue cycle management.
Most teams discover this during month three's revenue reconciliation when they realize 30% of eligible CCM charges never got billed. The technical fix—API connections between your chronic care management platform, billing system, and clearinghouse—takes weeks to implement properly.
RPM: Revenue Accelerator or Margin Killer?
Remote patient monitoring can add up to $91/patient/month alongside CCM—but only if you segregate minutes; you can’t count the same time twice. If you’re learning how to build a chronic care management app, treat RPM as a parallel service line with its own audit trail (think device event → review → documented action).
- Track separately, bill cleanly: A BP review may bill under RPM (e.g., 99457), while a med-adjustment conversation belongs to CCM (e.g., 99490).
- Prove every minute: High RPM growth has drawn scrutiny; your platform should output device-specific logs that attribute which minutes went where.
- When RPM hurts: In straightforward diabetes management, hardware, training, and support can outstrip the extra $43–$48/month, especially with low device adherence.
The Pharmacy Integration Nightmare
Multiple studies report ~25–27% of home medications go unrecorded at admission/transition—a reconciliation gap with clear safety and billing implications.
For CCM, this translates to:
- Care plans built on incomplete medication lists
- Duplicative prescriptions that trigger adverse events
- 42% of discharge medication orders containing errors, primarily from medications that should have been restarted but weren't
- Pharmacy claims data arriving 30-60 days late, making real-time adherence tracking impossible
The technical challenge compounds: Each pharmacy chain uses different data formats, update frequencies, and authentication protocols. Without unified pharmacy feeds, your care coordinators spend precious billable minutes calling pharmacies to verify fill dates instead of actually managing chronic conditions like hypertension.
Related: Pharmacy App Development Guide
Avoiding the Five Fatal CCM Development Mistakes
Skip these five traps when building a chronic care management platform, and you’ll avoid the graveyard of programs stuck with tiny patient panels and stagnant health outcomes.

Mistake #1: Building for Every Chronic Condition at Once
The teams that succeed start with diabetes, hypertension, or COPD—pick one, nail the workflows, then expand. Why? Each condition has unique care protocols, medication patterns, and escalation triggers.
Teams building for "all chronic conditions" ship generic tracking tools that satisfy no one. Your care coordinators need disease-specific decision trees, not a blank notes field. Focus on 2-3 conditions max where your providers already excel, then scale horizontally once you're billing consistently.
Mistake #2: Over-Engineering Care Plan Creation
Complex care plans reduce revenue, not increase it. Medicare requires a care plan, not a dissertation. The profitable platforms use simple templates with
- 5-7 standard goals
- medication lists
- basic preferences
Meanwhile, teams building 20-field intake forms with branching logic watch their care coordinators burn 45 minutes per patient just on setup.
With successful programs engaging patients 3+ times monthly, your care plan needs to enable quick updates, not academic perfection.
Mistake #3: Ignoring the Provider Workflow
Providers spend 20-30 minutes monthly on CCM documentation, but they touch your app during visits—where they have 5-7 minutes max. If your platform requires providers to navigate three screens to review care notes or approve plans, adoption dies.
Build for glanceable dashboards, one-click approvals, and automatic documentation that captures billable time without manual entry.
Mistake #4: Assuming Monthly Patient Engagement
Reality check: Most patients won't actively use your app monthly. The successful platforms flip the model by pushing
- automated check-ins
- medication reminders
- care coordinator outreach
rather than waiting for patient-initiated contact. Your engagement strategy should assume passive participation as the default, not the exception.
Mistake #5: Ignoring Care Coordinator Workflows
Care coordinators, not providers, drive CCM success. They're managing 200-500 patients monthly, making 20-minute documentation windows across multiple calls. If your platform doesn't have bulk actions, quick patient switching, and automated time tracking, you're building for the wrong user. Design for care coordinator efficiency first—provider oversight second.
The Real Cost Breakdown: MVP to Revenue Generation
When it comes to chronic care management software development, the single biggest mistake founders make is assuming an “MVP” is enough. In this space, a minimum viable product won’t even clear a compliance audit.
What you really need is a Minimum Billable Product—the leanest version of your app that can generate legitimate Medicare claims without triggering denials or clawbacks.
Phase 1: Minimum Billable Product ($150k–$250k)
At this stage, your (custom) build (from scratch) must include:
- Core CPT workflows with time-tracking, consent capture, and care plan documentation
- Immutable audit trail architecture—proving duration and scope of services
- Basic integrations with EHR/PM systems for patient rosters and billing handoffs
Think of this phase as the price of admission. Without it, you can’t even submit a compliant claim. Teams that try to cut corners here usually find themselves spending twice as much re-architecting later.
Phase 2: Scaling to Profitability ($100k–$150k)
Once you’ve proven compliance and billed a few cycles, the next investment is what pushes you into profitability:
- Automation layers: AI-assisted time categorization, auto-populated care plans, pharmacy reconciliation feeds
- Patient engagement tooling: structured symptom reports, consent acknowledgments, adherence workflows that double as billable events
- Team efficiency features: batch documentation, workload dashboards, and coordinator-centric interfaces
This is where your unit economics flip: a care team that can handle 400–500 patients per FTE instead of 150–200. That scale is what unlocks sustainable margin.
Hidden Costs You Can’t Ignore
Most founders underestimate the non-dev costs:
- Compliance audits: external validation of HIPAA, SOC 2, and CMS requirements ($25k–$50k per round).
- Security assessments: penetration testing, encryption validation, disaster recovery planning.
- Operational training: onboarding care coordinators and providers to workflows that stand up under audit pressure.
These aren’t “optional extras”—they’re the difference between keeping your reimbursements or watching them clawed back.
The APCM Wildcard: Build vs. Buy in 2025
The new APCM (Advanced Primary Care Management) program is a curveball. By expanding the reimbursable scope of longitudinal care, APCM blurs the line between CCM, RPM, and behavioral health integration. For builders, it means two things:
- Bigger upside if your platform can support multi-condition management across chronic conditions like heart disease, diabetes, and COPD.
- Greater complexity if you go custom—because the regulatory surface area just tripled.
This is where “buy vs. build” becomes existential. A platform that already ships with Medicare-compliant components and modular compliance engines can get you live in months, not years. Pure custom development? You’re likely looking at seven figures before profitability.
CCM Development Approaches
*Pessimistic Specode scenario with lots of customizations.
Bottom line: if your goal is a chronic care management application that generates revenue, budget realistically. $150k–$250k gets you in the game. Another $100k–$150k helps you scale. But the real cost of doing it wrong—missed compliance, failed audits, or rebuilds—is far higher than doing it right from day one.
How Specode Helps Accelerate CCM Platform Development
By this point, it’s clear that building a chronic care management app isn’t about features—it’s about billing-readiness, audit-proof documentation, and workflow efficiency. That’s where Specode changes the calculus.
Medicare-Ready from Day One
Specode is an automated platform with reusable, HIPAA-ready components—auth & roles, e-consent, audit logs, scheduling & telehealth, secure messaging, payments/claims, basic reporting, and EHR connectors—so you don’t rebuild the plumbing every CCM app needs. You assemble the common 80% and spend your time on the last-mile workflows that make your program different.
AI Builder: Build by Conversation, Not Tickets
Specode’s AI chat assistant assembles HIPAA-ready components into working CCM flows from plain-English prompts.
- scaffolds screens, APIs, and data models
- wires RBAC, e-consent, and audit logs by default
- pre-wires EHR paths (Canvas out-of-the-box; Epic/Oracle/athena scoped case-by-case)
You ship real, exportable code in your repo—no black boxes, no lock-in.
From 8 Weeks to Market
With Specode, founders can go live with a HIPAA-ready CCM platform in as little as 6–8 weeks. Compare that to the 9–18 months (and 2–3× the cost) of full custom development. Our approach has already powered launches like AlgoRX, which hit 7-figure ARR in under six months .
Future-Proofed for APCM
The 2025 APCM program expands the surface area of reimbursable longitudinal care. Specode’s modular architecture and API-first design mean you don’t just get a CCM app—you get a foundation that adapts to future Medicare models, whether that’s chronic conditions like heart disease or multi-condition bundles.
If your goal is to make a chronic care management app that generates revenue, Specode provides the shortest, safest path: pre-built compliance, faster time to market, and code ownership that grows with your business.
Start free on Specode—add CCM time tracking, audit-proof notes, and claims export; preview in minutes, iterate daily. Need EHR or pharmacy rails later? Step up to Custom and keep momentum without a rewrite.
Frequently asked questions
A compliant, revenue-ready CCM app typically requires $150k–$250k for a Minimum Billable Product and another $100k–$150k to scale profitably. Costs rise if you add advanced automation, multi-condition management, or deep EHR integrations, and compliance audits add ongoing expenses. Choose Specode to optimize your costs.
The main reason is that practices underestimate the operational burden of documentation, time tracking, and compliance. Without automation and audit-ready workflows, staff costs exceed reimbursement. Fewer than 3% of eligible practices run profitable programs because they launch with patient portals instead of billing-first platforms.
The essential features are audit-proof time tracking, care plan templates, medication reconciliation, and provider communication tools that capture billable time. Patient-friendly extras like reminders and messaging are useful only if they also generate documentation that supports Medicare billing.
Traditional custom builds can take 12–18 months to reach audit-ready status. With pre-built HIPAA-compliant components, teams can launch a CCM platform in 6–8 weeks, provided requirements are clear and integrations are scoped properly.
The new Advanced Primary Care Management program expands reimbursable scope across chronic conditions like heart disease and diabetes. This increases both the opportunity and complexity of development. A modular architecture with standardized APIs becomes critical, making platform assembly a more practical path than full custom builds.









