Knack for Healthcare Apps: When HIPAA Compliance Isn't Enough
Two platforms walk into a clinic.
Both promise “launch fast.” Only one survives audit season.
General builders are fantastic for dashboards and back-office CRUD. But the moment a clinician says “limit access to Patient 143 for Dr. Lee, delegate to her NP for 24 hours, log every touch, and write back to the EHR without nuking provenance,” the glue gun comes out. That’s where teams spend quarters duct-taping “features” into workflows.
- If your roadmap tops out at forms + tables, the general builder gets you there.
- If your roadmap includes eligibility, care plans, prior auth, eRx/labs, payer rules, and EHR write-backs, you need healthcare-native components and code ownership. That’s Specode.
Specode isn’t a blank canvas—it’s assembly: a basic EMR, audit-ready primitives, patient-scoped RBAC, and a sane path to integrations. The AI assistant doesn’t do magic; it turns your specs into working, billable flows you can actually defend—clinically and operationally.
Let’s compare where each platform shines—and where it quietly hands you a roll of duct tape.
Key Takeaways
- HIPAA is the floor. The cliffs are dynamic RBAC, immutable audit trails, prior-auth workflows, and safe EHR write-backs—areas where generic platforms stall.
- Assembly beats abstraction: reusable, healthcare-specific components with full code ownership outpace no/low-code once real clinical operations start.
- Specode’s AI assistant accelerates from spec to working healthcare app while preserving HIPAA-friendly defaults (encryption at rest/in transit, RBAC, audit logging) and an escape hatch you control.
Knack's HIPAA Package: What You Actually Get
Knack tries to be everything to everyone—CRM, portals, inventory, construction, government, healthcare. That breadth is fine for operations; it’s brittle for clinical apps. For healthcare, their HIPAA package is a hardening layer on a generic database builder.
Pricing Reality
HIPAA is available only on Enterprise; pricing isn’t publicly listed.
Knack HIPAA Package: Included vs Not
What You Still Have to Assemble
Knack gives you secure storage; you still build the care-delivery logic and regulated integrations yourself—and none of these are claimed as native HIPAA features on their pages:
- E-prescribing & ePA (NCPDP SCRIPT flows, EPCS 2-factor & ID proofing).
- Labs (HL7 v2 ORU, LOINC mapping, or FHIR Orders/Results).
- Eligibility/claims context (X12 270/271, payer rules feeding prior auth & billing).
- FHIR R4 endpoints: your integration targets (EHRs/payers) increasingly expect FHIR R4
What Their Own Stories Actually Show
- Amputee Associates: migrated from spreadsheets; eliminated “data overrides” and coordination chaos—operations, not eRx or lab routing.
- Arizona Autism: productivity tracking, nursing oversight, timesheets (with Twilio); migrated from Quickbase for cost/UI—again, operations over clinical integrations.
HIPAA gets you past the bouncer; it doesn’t teach the band to play. Knack’s Enterprise layer checks the right boxes—BAA, encrypted hosting, stricter session rules—and that’s valuable. But if your roadmap includes e-prescribing, labs, eligibility, prior auth, or anything that smells like care delivery, you’re not shopping for a database—you’re buying down operational risk. And assembling that from generic parts is where teams lose months and momentum.
The Healthcare Gap: What HIPAA Compliance Doesn’t Solve
Clinical operations are exception-driven—insurance flips mid-visit, prior auths bounce, licenses lapse. Database-first tools crack when workflows branch by payer, diagnosis, or state rule.
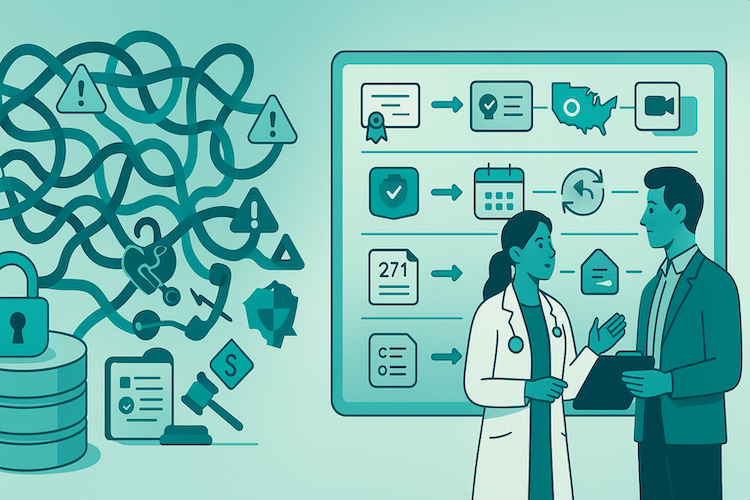
Where Generic Platforms Break
Generic platforms handle storage; the failure mode is orchestration.
- Credentialing & monitoring: Primary-source checks (boards, schools, cert bodies), DEA where applicable, OIG/state sanctions, malpractice coverage, renewal calendars. Storing fields is easy; orchestrating verifications, re-cred timers, and sanctions alerts is not.
- Telehealth beyond video:
- Adaptive quality + audit trails that survive bad bandwidth.
- In-visit tools: pull PACS images, labs, med histories; document with structured data.
- State overlays: consent/recording rules, cross-border prescribing limits, per-state policies.
- Eligibility (X12 270/271) reality: Transform payloads, juggle payer endpoints/auth, parse 271 responses and AAA rejections, handle retries/timeouts. It’s orchestration, not a single REST call.
- Medicare/Medicaid billing logic: Time-based programs (e.g., chronic care, remote monitoring), device-use thresholds, modifier rules, and place-of-service impacts. Prevent double-billing, enforce diagnosis/code pairing, and produce resubmission logic when denials hit.
Real Implementation Walls: Where Knack Healthcare Projects Struggle
Knack is fine for calendars and CRUD. Healthcare isn’t. The moment you plug into the real ecosystem—e-prescribing, labs, multi-provider ops—generic templates and connectors buckle.
E-prescribing: standards, identity proofing, audits
What sounds like “send a script” is a regulated relay:
- Standards stack: NCPDP SCRIPT (current spec, mandated timeline baked in) plus formulary/benefit checks across plan rules.
- Controlled substances (EPCS): identity proofing, two-factor credentials, tamper-evident audit trails.
- Modern endpoints: real-time prescription benefit via FHIR with stricter auth/token flows.
Why this breaks on generic tools: you’re hand-rolling message validators, credential lifecycles, and immutable logging on a database builder.
Labs: HL7/FHIR is not “just JSON”
Lab data is opinionated and unforgiving:
- HL7 v2 ORU: OBR/OBX/NTE segments, delimiters, amendments, critical values, ACKs.
- FHIR R4 adoption rising: orders/results, LOINC mapping, multi-lab quirks.
Where it stalls: edge cases (multi-part results, corrections, STAT alerts) demand a parser + event engine, not formula fields.
Multi-provider coordination needs healthcare-grade RBAC
Roles aren’t “admin/user.” Daily reality:
- Weekend coverage with time-boxed, patient-scoped access.
- Resident notes requiring attending co-signature.
- Billing visibility without exposing psychotherapy notes (42 CFR Part 2).
Gap: static roles ≠ dynamic, context-aware permissions.
Cures Act patient access: “immediate” isn’t a toggle
Patients must see their information without artificial delay. The gotchas:
- Results often release before clinician review; state carve-outs vary.
- You owe granular access logs (who saw what, when).
Need: policy-aware release workflows + audit trails, not a checkbox.
Prior authorization: payers’ maze, your headache
Where projects really stall:
- Moving parts: payer-specific rules, clinical attachments, live status feeds, denials → appeals.
- APIs: FHIR-based PA with defined turnaround clocks for urgent requests.
Reality on generic stacks: elaborate forms + manual portal checks—no rules engine, no automated resubmits, no closed loop.
These are orchestration problems with external dependencies. If your stack can’t natively handle them, velocity collapses as you scale.
The Hidden Costs of Generic Platform Healthcare Builds
You don’t buy a “HIPAA plan”; you buy a stack you can operate. With generic platforms, the bill shows up in layers you didn’t scope.
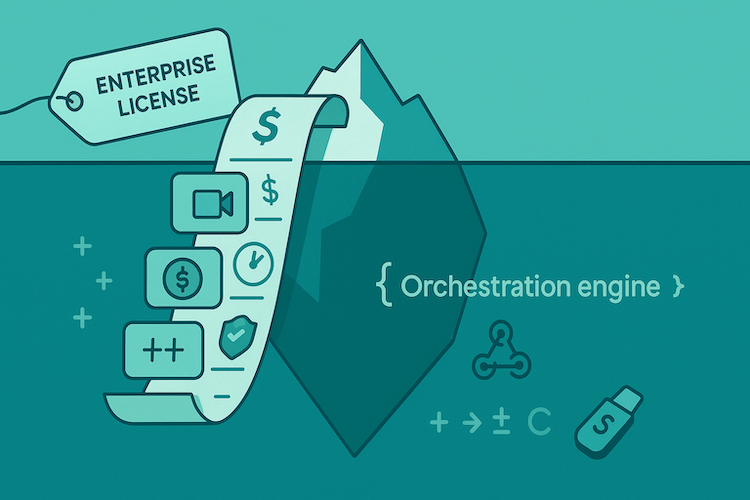
1) Enterprise plan ≠ total cost
The sticker price is the floor, not the ceiling.
- License delta: HIPAA lives behind Enterprise. Add-ons and higher API limits follow.
- Healthcare plugins: video, SMS, file storage, document signing—each is “just one more” fee.
- Custom code tax: anything clinical (eRx, labs, eligibility, PA logic) means JavaScript glue, webhooks, and external orchestration.
Net: Budget for the platform, then budget again for the parts that actually deliver care.
2) Developer hours to fight healthcare edge cases
The real spend is time—on problems the tool wasn’t built to solve.
- Workarounds on repeat: patient-scoped RBAC, time-boxed privileges, tamper-evident audit trails.
- Parser land: HL7/FHIR transforms, PA attachments, 270/271 eligibility handling, retries/AAA codes.
- Maintenance tail: every payer or lab tweak = another patch. The curve is not linear.
Net: You’re not “configuring”; you’re building an orchestration engine in the comments.
3) Third-party services to fill the gaps
Each plug-in solves a slice—and adds a new failure mode.
- Telehealth: video, waiting rooms, consent/recording, audit events.
- Payments: PCI scope, card vaulting, HSA/FSA quirks, dispute packs.
- Scheduling/Comms: live availability, reminders, PHI-safe templates, SMS/email failover.
Net: Costs, rate limits, and incident chains stack—coordination becomes your unpaid product.
4) Compliance consulting you didn’t plan for
BAAs are paperwork; compliance is product.
- Policy → code: minimum-necessary, access logging, retention/deletion, breach workflows.
- State overlays: consent/recording rules, 42 CFR Part 2 separations, minor access.
Net: Governance becomes feature work—someone has to own it release by release.
5) Migration when the ceiling appears
Prototypes feel fine—until concurrency and audits hit.
- Reality check: multi-role workflows and audit depth expose hard limits at scale.
- Rewrite in flight: exports, credential migrations, payer re-onboarding, retraining.
- True cost: the new build is expensive; the lost months are worse.
Net: Plan for a bridge or plan for a rebuild—pretending you won’t need one is the costliest choice.
A Quick, Honest TCO Frame
- TCO = Enterprise license
+ Third-party fees
+ Dev hours (build + integration + maintenance)
+ Compliance/QA cycles
+ Migration contingency.
If answers to immutable audits, eligibility parsing, patient-scoped access, retry logic are fuzzy, you’re not comparing prices—you’re comparing run-rate risk. The invoice for generic stacks arrives as schedule slip, brittle workarounds, and, eventually, a rebuild.
When Knack Works for Healthcare Use Cases
Knack shines when the job is structured data + internal ops, not regulated care delivery.
Internal Quality/Ops Dashboards
Great for consolidating multi-site metrics, productivity, schedules, claims status snapshots—i.e., replacing spreadsheet chaos with a governed portal. Arizona Autism uses Knack for staff productivity tracking and timekeeping (Twilio check-ins → timesheets). That’s ops, not eRx.
Research Data Collection and Registries
Good fit for tissue/sample inventories, consent-bounded access, and research collaboration—think anonymized/aggregated data access, not clinical ordering. Royal Free London/UCL built a system to manage tissue samples and share data with researchers; speed and access improved, but it’s data management, not a lab interface.
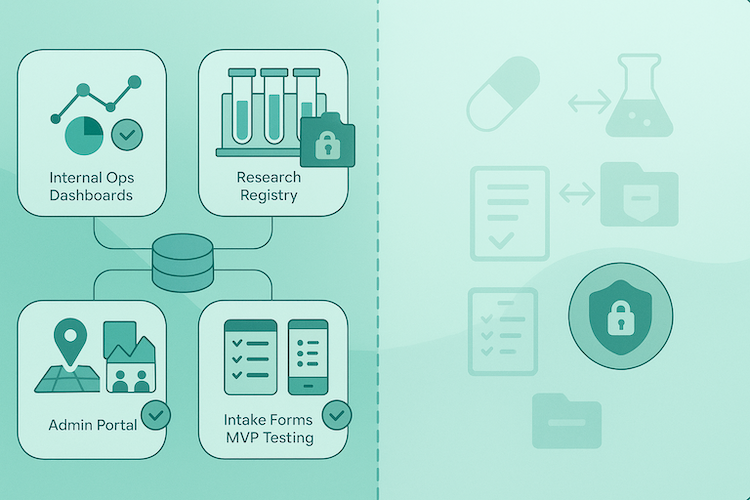
Multi-Clinic Admin Portals and Basic Patient Records
Solid upgrade from spreadsheets for multi-location coordination, appointments, and vetted record access. Amputee Associates moved from sheets to a unified app for patient info and scheduling coordination; the value was eliminating “data overrides,” not wiring to payers or pharmacies.
Intake Forms for Small Practices
Templates + forms + lists = quick wins for intake, simple triage, and handoffs—especially where you don’t need eligibility, prior auth, or device data. Knack’s healthcare page pushes patient portals and care-management templates, but it’s still database-first (no native eRx/labs).
MVP Testing Before a Production Build
Useful as a learning MVP to validate workflow and UI with real staff—cheap, fast, reversible. Once you need regulated rails (eRx, HL7/FHIR orders/results, X12 eligibility), you’re out of template territory. Knack’s HIPAA package emphasizes hosting, logging, encryption, and timeouts—not clinical integrations.
Quick Rule of Thumb
If success = replace spreadsheets, centralize ops, report on data, Knack fits. If success = deliver care (e-prescribing, lab ordering/results, payer exchanges, Cures-compliant patient access), you’ve crossed from database building into healthcare orchestration—and that’s beyond what Knack advertises.
Component Assembly vs. Database Building for Healthcare
Knack lets you model tables and slap forms on top. That’s database building. Healthcare, though, isn’t a contact list with PHI stickers—it’s a maze of workflows, exceptions, and regulated endpoints. You don’t need more tables; you need components built for care delivery.

Assembly: How Healthcare Actually Ships
With component assembly, you’re not inventing schema from scratch—you’re wiring pre-built, HIPAA-ready modules that already know what “chronic care time tracking” or “patient e-consent” looks like. The AI assistant stitches the flows, engineers refine edge cases, and you launch on rails paved by a decade of healthcare builds.
Database-First: Reinventing the Plumbing
Generic platforms force you into object-making theater:
- New schema for every workflow.
- Custom JavaScript for every eligibility or billing rule.
- DIY logging and auditing to satisfy compliance.
That’s not “configuring a platform”; that’s hand-rolling middleware in a drag-and-drop UI.
Side-by-Side Reality Check
Speed, Ramp-Up, and Extensibility
You don’t just “use” a generic platform—you learn it first.
- Knack (real ramp): Yes, there are healthcare-ish templates (e.g., practice management), role-based views (doctor/patient/owner), and a no-code Tasks automations UI. But to ship anything beyond CRUD you still have to internalize: the data object model, view/permission graph, formula logic, Tasks triggers, deployment constraints for the HIPAA plan, and where custom JS/webhooks start. That learning curve eats weeks before you even touch clinical edge cases.
- Specode (build flow): You describe the outcome in plain English; the AI assistant scaffolds screens, data models, and wires HIPAA-ready components (Intake Forms with branching + pre-auth, Provider Profile with credential fields, Telehealth with waiting room & notes). Engineers tighten the edges; you keep code ownership and can extend or swap modules as you grow.
Ramp time compounds. If your team spends cycles mastering a platform’s internals, you delay care workflows. Natural-language assembly flips that: days to working flow instead of weeks to workable scaffolding.
Bottom line: Healthcare isn’t about “storing data.” It’s about enabling care delivery. Assembly treats clinical patterns as first-class citizens. Database builders treat them like exotic hacks. Guess which one holds when you scale past the prototype?
Making the Platform Decision: Key Evaluation Criteria
You’re not picking a tool; you’re picking your next 18 months. Use this as a one-screen checklist you can hand to your team.
1) Map Your 18-Month Reality
- Roadmap: eRx, labs, eligibility/X12, prior auth, Cures-compliant patient access, multi-role RBAC, audit/retention.
- Traffic: expected DAU, concurrent visits, read/write mix, burst patterns (campaigns, flu season).
- Data gravity: which systems are source-of-truth vs derived (EHR, PM, pharmacy, lab, payer).
2) Integration Requirements
- Targets: EHR (FHIR R4), labs (HL7 v2/FHIR), pharmacy/eRx (NCPDP/EPCS), payers (X12 270/271, PA).
- Depth: read-only vs write-back; sync vs event-driven; attachment handling (PA docs, PDFs, images).
- Auth model: OAuth2/SMART-on-FHIR, key rotation, token lifetimes, re-auth patterns.
- Ownership: who runs the adapters, monitors failures, and fixes schema drifts?
3) Security, Audit, and Governance
- Access controls: patient-scoped, time-boxed, context-aware permissions; co-signature rules.
- Auditability: immutable trails (reads/writes/exports), admin actions, retention + deletion policies.
- Breach/IR playbooks: event capture, evidence packs, notification triggers, simulation frequency.
4) Operational Fit
- Ramp time: weeks to grok platform internals vs days to ship flows.
- Team shape: can product/ops drive changes without a platform specialist?
- Change cadence: how safely can you ship weekly (feature flags, sandbox data, rollbacks)?
5) TCO and Runway Risk
- TCO = license + third-party fees + integration build/maint + compliance/QA + migration contingency.
- Ceiling test: what happens at 50–100 DAU with multi-role workflows and deep audits?
- Latency to value: time to first reimbursable workflow (not “hello world”).
6) Code Ownership and Exit
- Repo & rights: do you own the code, infra config, and IaC?
- Escape hatch: how painful is swapping an integration or moving off platform entirely?
- Data portability: export format, re-import plan, downtime window.
Mini Decision Tree
- Need regulated rails in v1 (eRx/labs/eligibility/PA)? → Choose component assembly.
- Expect payer/EHR/lab growth or frequent rule changes? → Choose component assembly.
- All-ops, no regulated integrations (dashboards, intake, internal portals)? → Knack can fit.
- Learning MVP only, plan to rebuild later? → Knack for validation, budget migration.
Pick the path that minimizes orchestration risk across your roadmap—not the path that looks cheapest on slide two of the demo.
How Specode Delivers What Knack’s HIPAA Package Can’t
Knack hardens a database. Specode assembles a clinic. Here’s the delta that actually moves your roadmap.

Pre-Built Clinical Workflows
You start from working healthcare primitives—then tailor. Examples:
- Intake Forms with branching and pre-auth hooks
- Telehealth with waiting room + note linking
- Scheduling with live slots
- Provider Profile with credential fields
- Basic EMR with SOAP notes and an immutable trail
- Notifications with HIPAA-safe templates
You wire these (and many other) components; you don’t reinvent them.
Integration Stance That Matches Reality
Specode ships a Basic EMR foundation. If you need a full EHR, we can bootstrap Canvas Medical; Epic/Cerner/etc. are handled case-by-case via native APIs or middleware. eRx/labs/wearables are via partner integrations—not claimed as universal out-of-the-box. Translation: honest scope, clear path.
An AI Assistant Trained on Healthcare Patterns
Describe the outcome in plain English; the assistant scaffolds screens, data models, and wires components with HIPAA-friendly defaults. Keep iterating in convo, then drop to code when you want.
Code You Own, an Escape Hatch You Control
This isn’t a walled garden. You own the repo, extend modules, swap integrations, deploy to your infra—no rewrite tax when you grow.
Proof in Market: AlgoRX
Medication storefront + eligibility + provider automation + multi-pharmacy routing. Result:
- $1M+ in sales by month two and 7-figure ARR within six months
- ~12× ROI credited to Specode’s component approach
That flow would require heavy custom workarounds on a generic DB builder.
If your goal is care delivery, not just data storage, Specode’s component assembly + AI build flow gives you production-grade velocity now, and code ownership for whatever’s next.
If “HIPAA-ready” still leaves you stitching workflows by hand, try Specode. Open a free workspace, ask for “intake with consent + role-scoped messaging,” preview in minutes—then connect your EHR when you’re ready.
Frequently asked questions
Yes, but expect real rework. Typical steps: freeze schema, export data, map to healthcare-oriented models, rebuild role/permission logic, and re-implement integrations with auditability. It’s feasible, and we help teams do it, but total effort is usually higher than starting with code ownership and healthcare-native components.
Yes. You own the generated code and infrastructure templates, with no platform lock-in. Third-party services (e.g., eligibility, eRx, payments) remain under their own licenses; you can swap them without rewriting the core app.
Specode includes a basic EMR for typical workflows. We provide a bootstrap path to Canvas Medical and integrate others (e.g., Epic, Cerner) case-by-case via native APIs or middleware. eRx and lab ordering are supported through partners. This keeps you flexible while avoiding bespoke plumbing from scratch.
Generated projects default to encryption at rest and in transit, RBAC, audit logs, and environment separation. These are starting points, not a substitute for your own security review and BAAs. For formal security documentation and current architecture specifics, request the latest materials from the Specode team.
No. Specode is code-first assembly with reusable, healthcare-specific components and an AI assistant to accelerate development. You keep full code ownership, get deeper clinical primitives, and integrate on your terms. General builders optimize for speed to CRUD; Specode optimizes for durable, auditable healthcare operations.









