Managing Medical Cannabis Patient Journeys: Compliance & Care Coordination
Most medical cannabis platforms fail for a boring reason: they try to scale like dispensary apps. But once you’re dealing with diagnoses, dosing trajectories, registries, provider roles, and 40-plus rulebooks, you’re no longer in retail—you’re operating a clinical system with cannabis-specific constraints.
This guide reframes the whole stack: patient journey, provider workflows, dosing engines, multi-state rule models, and compliance architecture built to survive the next regulatory plot twist, not just the next release cycle.
Key Takeaways
1. Medical cannabis isn’t a shopping flow—it’s a longitudinal care pathway.
Platforms that don’t support N-of-1 dosing, validated PROs, and structured follow-up bleed users long before outcomes emerge.
2. Provider workflows determine adoption—not strain menus or dashboards.
State-aware credentialing, repeatable intake → recommendation → monitoring loops, and audit-ready documentation make cannabis feel like a therapy clinicians already manage.
3. Multi-state scalability is a rules-engine problem, not a product sprint problem.
Fragmentation lives in configuration—eligibility, roles, registry steps, documentation—not in forks, branches, and “we’ll fix that for State #4.”
Why Medical Cannabis Platforms Aren’t Dispensary Apps
Medical cannabis isn’t a prettier weed menu with a green cross slapped on top. If you treat it that way, you don’t just leave outcomes on the table—you walk straight into regulatory and clinical risk.
A medical cannabis platform lives in the same world as EHRs, care pathways, and quality metrics. Dispensary apps live in the world of carts, coupons, and store traffic.
The Regulatory Reality: Forty-Plus Jurisdictions, Not One Market
As of mid-2025, roughly forty-plus U.S. states, D.C., and several territories run their own medical programs—with different qualifying conditions, registries, purchase caps, record-keeping rules, and enforcement agencies layered on top of local ordinances.
You’re not building for “the U.S. market,” you’re building for dozens of slightly incompatible rulebooks at once. If your architecture doesn’t assume that fragmentation from day one, you’ll hard-code your way into a corner and pay replatform tax the moment you expand or a state updates its rules.
What Cannabis Dispensary Software Actually Solves
Cannabis dispensary software is built to keep a retail operation out of trouble with state cannabis regulations while moving product efficiently. Its job description is pretty specific:
- Track inventory and plant lifecycle
- Enforce purchase limits and age verification
- Push mandatory events into the state’s tracking system
- Run point-of-sale and basic loyalty/marketing
Systems like Metrc, used in states such as New York, Oklahoma, and many others, are explicitly designed as seed to sale tracking tools: they monitor plant actions, inventory movements, and sales data so regulators can see exactly what happened to every gram.
That’s what most “cannabis POS + compliance” stacks are optimized for—not for clinical outcomes, longitudinal care, or cross-provider coordination.
So if your functional spec reads like:
“Menu → cart → checkout → send required data to state tracking system”
…then yes, you’re in dispensary-app territory.
Why Medical Platforms Need Clinical, Not Just Commercial, Workflows
A serious medical program needs something much closer to medical marijuana software or even a lightweight cannabis EMR than a retail POS.
At minimum, you’re dealing with:
- Clinical intake (diagnosis, comorbidities, contraindications, meds)
- Provider recommendations (product type, THC/CBD ratio, route, initial dose)
- Ongoing symptom and side-effect tracking
- Adverse-event capture and follow-up
- Longitudinal outcome data by indication, dose, and formulation
The research ecosystem around cannabis apps actually reinforces this gap: content analyses of cannabis-related mobile apps on iOS and Android found that most focused on strain information, dispensary locations, or recreational content, with almost none built as evidence-based tools for treatment or cessation.
That’s exactly what you’d expect when teams start from “let’s build a cool weed app” instead of “let’s manage a chronic pain or epilepsy cohort over 12–18 months.”
Once you’re storing clinical histories and outcomes, you’re no longer just a shop—you’re edging into “covered entity or business associate” territory. At that point, you’re operating a HIPAA compliant cannabis app whether you like it or not:
- You need clear PHI boundaries and role-based access
- You need audit logs for who saw what, and when
- You need breach-notification and data-retention policies that survive discovery
Architecturally, that’s an EMR-adjacent problem with cannabis-specific constraints, not a fancier e-commerce problem.
The short version: if your roadmap includes physician recommendations, state registries, and multi-visit titration, you’re already in platform territory. Treat it like health tech from day one—or plan for an expensive do-over when the regulators, payers, or investors start asking EMR-level questions.
If you’re thinking about how your medical cannabis platform crosses into PHI territory, it’s worth revisiting what a real HIPAA compliance in no/low-code environment looks like. It’s a concise breakdown of safeguards, boundaries, and pitfalls teams hit when they underestimate compliance debt — especially relevant once you’re storing diagnoses, outcomes, or provider recommendations.
The Patient Journey Architecture That Drives Adoption
Why Operators Struggle With the Patient Journey
Most operators don’t lose patients because cannabis “doesn’t work”—they lose them because the workflow looks like a shopping flow, not a care pathway.
Clinician surveys show the same pattern:
- ~58% believe medical cannabis has therapeutic value.
- ~36% lack confidence discussing risks/benefits.
- ~85% want more education.
Clinicians believe in the therapy but lack dosing, interaction, and monitoring guidance. Patients then default to Reddit, budtenders, and “strain review” apps—turning medical workflows into e-commerce patterns and tanking treatment adherence.
A real platform isn’t “dispensary software with a medical badge.” It behaves like a disease-management tool that uses cannabinoids as the intervention.
The N-of-1 Titration Model, Not “Pick a Strain”
Treat cannabis like “pick a strain” and you’ve lost before you start. Evidence is patchy, THC/CBD ratios are condition-specific, and clinicians must run N-of-1 experiments:
- Start low.
- Adjust ratio and route gradually.
- Track outcomes over weeks.
- Lock in what works for this patient.
Data backs this: a New York study found six distinct THC/CBD dosing trajectories—different patterns for chronic pain, cancer, neuropathy, epilepsy, and “high-then-taper” users. This is why indica/sativa UX is useless; dosing needs differ from day one.
Your platform must treat every patient as an N-of-1 trial and your titration workflow as the protocol engine.
What a Structured Cannabis Care Pathway Actually Looks Like
A platform that drives outcomes begins with clinical context and ends with structured PROs.
A modern pathway includes:
- Baseline Assessment — diagnosis, severity, comorbidities, contraindications.
- Condition-Specific Intake — forms tailored to chronic pain, epilepsy, neuropathic pain, oncology; validated instruments auto-loaded.
- Onboarding & Consultation — med review, interaction screening, expectation setting.
- Initial Recommendation — route selection (vaporized for flares, oral/sublingual for baseline control); THC/CBD ratio based on indication.
- Symptom Tracking & PROs — dose, timing, route, formulation logged; validated PROs; nudges at clinically meaningful intervals.
- Follow-Up Triggers (1–6 Months) — 1–3 months for high-risk patients; 3–6 months for stable users; triggered visits when PROs worsen or adherence drops.
- Dosage Adjustment Workflows — provider reviews longitudinal data, adjusts dose/ratio/route, and pushes updated plans to the patient app.
If your platform can’t run this loop end-to-end, it’s not a medical platform—it’s a dressed-up point-of-sale.
The Adoption Leak: When You Don’t Track Outcomes
The numbers are brutal:
- 57.9% of chronic musculoskeletal pain patients discontinue within 12 months.
- 44.7% quit in the first three months.
But supervised medical-cannabis registries with structured follow-up show dramatically better results—one Israeli registry reported:
- 89.7% in active treatment at one month
- 70.6% meeting success criteria at six months
The pattern:
- Unstructured use → high early discontinuation
- Structured care + PROs + clinician oversight → far higher retention + improvement
If your platform lacks PROs, symptom tracking, and closed-loop feedback, you’re effectively telling patients: “If it doesn’t work, figure it out yourself.”
That’s how interest turns into churn.
The fix isn’t more marketing—it’s architecture. Build the journey around titration and outcomes, and adoption takes care of itself.
Any team dealing with multi-state rules should understand the architectural patterns behind the leanest stack to build health apps. It covers the infrastructure, integration boundaries, and component choices that prevent regulatory logic from leaking into core code — exactly the kind of discipline multi-state cannabis operators end up needing.
Scaling the Dosage Optimization Workflow
You’ve already accepted that every patient is an N-of-1 titration trial. Scaling that across thousands of patients, dozens of conditions, and constantly shifting formulations is where platforms either become clinical infrastructure—or quietly prove they were just dispensary tooling with extra fields.

Why Dosing Optimization Breaks Most Platforms
Most cannabis software systems store products as SKUs, not interventions. Platforms fail because they don’t treat dosing as a living protocol. Once you support more than a handful of patients, spreadsheets and free-text notes collapse. You need a dosing architecture that behaves more like clinical decision support.
Designing a Dosing Engine With Clinical Rigor
A scalable cannabis dosing engine borrows from pain-management software, behavioral-health tracking, and disease-management programs. At minimum, it should be able to:
- Capture clinical context as structured fields: indication (fibromyalgia vs cancer pain vs epilepsy), onset expectations (oral vs sublingual vs inhaled), contraindications (cardiac risk, psych history, sedating meds), co-medications.
- Encode route and formulation explicitly: full-spectrum tincture vs vaporized flower vs softgel vs sublingual, plus oral/inhaled/transdermal/sublingual flags.
- Track dose details in mg for THC, CBD, and relevant minor cannabinoids so “10 mg didn’t work” isn’t just narrative.
- Store timing patterns (AM/PM, scheduled vs PRN) to distinguish protocol failures from simple schedule mismatch.
- Log contextual factors (sleep, stress, menstrual cycle, alcohol use, etc.) alongside each dosing event.
- Capture short-interval outcomes (e.g., pain at 20 min for vaporized doses, 120 min for oral) so you can model onset and peak, not just daily averages.
- Run trajectory analytics by clustering patient journeys by condition + formulation + outcomes instead of treating each patient as a blank slate.
- Detect tolerance and risk patterns (flatlining improvement at stable dosing, rapid escalation, adherence drift) and surface them proactively.
- Suggest next-step adjustments (e.g., alternative routes for breakthrough pain, different formulations after adverse responses) within approved ranges.
- Flag anomalies like worsening anxiety with THC-heavy titration or seizure spikes after formulation switches, where manual review is mandatory.
This is where AI actually earns its keep: not by “picking a strain,” but by pattern-matching hundreds of thousands of structured dosing instances to propose what’s most likely to work next.
Operational Patterns That Make Dosing Scalable
The engine only matters if the workflows around it scale with real clinics:
- Standardized follow-up cadence baked in: high-risk / complex patients on 4–6 week cadence, stable chronic cases on 10–12 weeks, protocol-driven indications (e.g., epilepsy) tied to seizure or symptom logs—enforced by the platform, not sticky notes.
- Configurable threshold alerts that trigger review when improvement plateaus 10–14 days, side effects cross tolerability limits, adherence becomes erratic, or dosing escalates quickly—with definitions tuned per condition/service line (oncology vs chronic pain vs neurology).
- Provider-ready summaries instead of diaries: a dashboard that compresses 30–90 days into a dose–response curve, flags crossed thresholds, suggests next titration steps inside approved bands, surfaces interaction risks, and produces audit-ready documentation of every adjustment.
If the “dosing dashboard” still feels like reading a diary instead of a clinical report, it isn’t scalable—no matter how good the underlying engine is.
The Scaling Principle: Dosing Is a System, Not a Sidebar
Most operators try to “add dosing features.” That’s backwards.
Dosing is the platform:
- It drives clinical value
- It determines retention curves
- It generates the longitudinal data investors and clinicians care about
- It forms the backbone of provider trust
If your architecture treats dosing like a supplemental module instead of the operating system for the entire patient experience, you won’t scale beyond a single clinic—or a single state.
The operators who win treat dosing as a core data model, a workflow engine, and a clinical feedback loop all at once. Everyone else discovers too late that their “dosing feature” needed to be the architecture.
If you want context on how Specode approaches healthcare-grade scaffolding beyond cannabis, the healthcare app builder guide shows how clinical data models, HIPAA-ready components, and workflow engines come together. It’s the broader backdrop behind the architecture you’re seeing in this cannabis-specific deep dive.
Provider Integration and Clinical Workflows
If the patient journey is the front stage, providers are the backstage crew keeping the whole thing upright. Ignore how clinicians actually work and you get low adoption, passive-aggressive feedback, and dosing notes buried in someone’s personal Excel file.
The Provider Education Gap You Must Design Around
Most clinicians believe medical cannabis can help—but lack dose tables, guidelines, and monitoring playbooks. Your platform’s job isn’t to turn them into strain experts; it’s to make cannabis feel like any other complex therapy:
- Structured, condition-aware intake
- Pragmatic protocol suggestions within safe ranges
- Documentation that fits existing note patterns
- Decision support that highlights risk and trajectory, not pseudo-insights
Design for this and cannabis becomes manageable. Ignore it and you become a side-portal.
Credential Management: Who Can Do What, Where
You need state-aware provider profiles, not one generic role.
State-Aware Profiles
- License type, issuing board, jurisdictions
- Active/inactive status, renewal dates
- Role mapping (“may certify,” “counsel only,” “view-only”)
State Policy in Data, Not Code
- Per-state policy tables defining who can act
- Centralized rules so adding a state doesn’t require workflow rewrites
Automated Guardrails
- Block flows when licenses lapse
- Restrict high-risk actions to specific roles
- Clear explanations when actions are denied
If you can’t answer “who is allowed to click this here, and why,” you don’t have real credential management.
Intake and Recommendation: From Chaos to Repeatable Protocol
Providers want a structured, 15-minute workflow, not a “cannabis tab.”
Pre-Visit Intake
- History, symptoms, contraindications auto-surfaced
Visit Workspace
- Risk factors highlighted
- Condition-specific dose ranges, routes, THC/CBD bands
Recommendation Composer
- Indication(s), route, starting dose, schedule
- Links to product abstractions that survive SKU changes
Patient-Facing Summary
- Plain-language plan: what to take, when, what to watch for
Every step should produce structured data and a narrative note.
Ongoing Monitoring: Dashboards That Earn Their Space
Dashboards must behave like decision consoles:
Cohort View
- Who’s improving, flat, deteriorating
- Filters by condition, product family, route, provider
Per-Patient View
- Symptom trajectories vs dose changes
- Adherence + timing patterns
- Side-effect frequency and severity
AE Tracking (Mandatory)
- Structured AE logs
- Provider triage (expected / adjust / escalate)
- Logged follow-up actions
Alerts & Tasking
- Triggers for AE severity, dose escalation, worsening PROs
- Routed to the right role; visible until resolved
If clinicians need five screens to decode a patient’s status, your platform isn’t integrated.
Cross-State Coordination: Because Patients Move
Your system must handle:
Jurisdiction-Aware Episodes
- Each tied to a state’s rule set + provider credentials
Transition Workflows
- Close old episode
- Re-onboard under new eligibility/registry rules
- Transfer relevant history within local constraints
Referral / Hand-Off
- Secure sharing of history and outcomes
- Full audit logs of access
If this flow relies on emailed PDFs, scalability is already broken.
Documentation and Compliance: If It’s Not Logged, It Didn’t Happen
A HIPAA-grade workflow requires:
Atomic, Auditable Actions
- Certifications, recommendations, dose changes
- AE reviews, consent + data-sharing events
Immutable Audit Trail
- Who did what, when, under which role
- Before/after values for key fields
Compliant Exports
- Machine-readable regulator feeds
- Human-readable summaries for EMRs/legal files
Logs must tell a defensible clinical story—not just exist.
The Integration Rule of Thumb
If clinicians must mentally switch into “cannabis mode,” adoption dies. Treat cannabis like any other high-variance therapy:
- Integrated scheduling
- Integrated intake and decision support
- Integrated documentation and follow-up
Do that, and provider workflows stop being the bottleneck—and start being your advantage.
For teams optimizing speed without compromising compliance, the quickly launch a health app walkthrough illustrates the 0→1 motion: small prompts, fast iteration loops, and guardrails that mirror the same patterns needed for cannabis dosing, PROs, and clinician workflows.
State Compliance Requirements: The Fragmentation Problem
You’re not “just” doing medical cannabis compliance—you’re building software that has to survive 50-state politics, federal ambiguity, HIPAA, and seed-to-sale rules without collapsing into if-else spaghetti. Get this wrong and you don’t just pay a lawyer tax—you ship an unmaintainable codebase and block launches. This is the fragmentation problem.
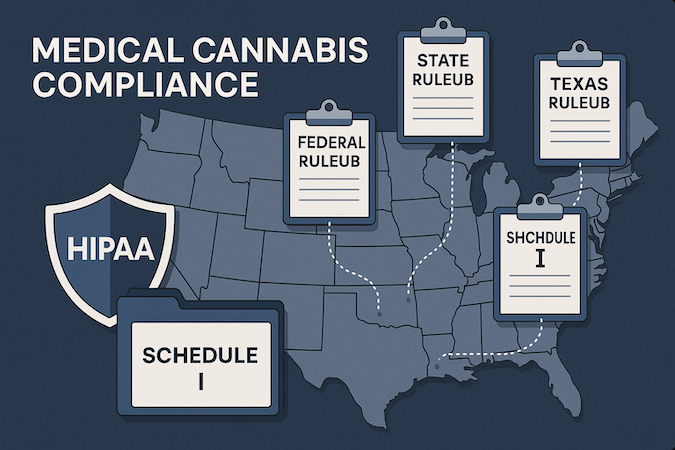
Federal Schedule I and State Labs: 40 Different Rulebooks
Federally, cannabis is still Schedule I—“high abuse potential, no accepted medical use.” States have built workarounds, resulting in:
- 40 states + three territories + D.C. with medical programs
- 24 states with adult-use layered on top
Each jurisdiction defines its own:
- Qualifying conditions
- Purchase caps and dosage/product rules
- Reporting schedules and audits
- Data retention and access policies
Enforcement varies (cannabis boards, DOH, agriculture), with municipalities adding zoning and operating constraints. That’s not a checklist—it’s a mini-rules engine per state. “Medical cannabis compliance” is really dozens of overlapping regulations sitting on a Schedule I foundation.
Four Compliance Layers You Can’t Treat as Edge Cases
Treat these as afterthoughts and you’ll rewrite core workflows for every new state.
1. Patient Registry: Who Qualifies, and How You Prove It
Most states run a cannabis patient registry:
- Certification → active patient record
- Central databases tracking cards/recommendations
- Some split “full” vs “low-THC/high-CBD” access
Platform implications:
- You’re handling PHI: identity, condition, certification
- Registry IDs may need syncing
- Retention and re-certification rules vary
“Medical marijuana onboarding” is a state-aware eligibility + registry-sync workflow, not a form.
2. Product Tracking: Seed-to-Sale Meets Care Pathways
Many states mandate Metrc or BioTrack. Metrc tracks plants/products from seed to sale (harvests, transfers, tests, retail events) across numerous jurisdictions.
For your platform:
- Clinical recommendations must map cleanly to SKUs/lots
- Internal dosing abstractions can’t break state reporting
- Switching vendors (Metrc → another STS) shouldn’t blow up APIs
This isn’t “METRC integration”; it’s a core contract between clinical workflows and compliance.
3. HIPAA Overlap: When Cannabis Data Becomes PHI
Some argue dispensaries aren’t HIPAA covered entities; others note that once you store diagnoses, prescriptions, or insurance, HIPAA standards apply.
Once you:
- Store diagnosis/treatment
- Track longitudinal outcomes
- Exchange data with clinicians or payers
…you need administrative, technical, and physical safeguards (BAAs, encryption, access control, audit logs). If your roadmap includes provider dashboards or adverse-event tracking, treat yourself as HIPAA-grade from day one.
4. Provider Credentialing: The Rules Aren’t Uniform
States define roles differently. Example: Washington’s Medical Cannabis Consultant requires DOH-approved training, CPR, and background checks. Others rely on physicians or NPs with varying documentation and CE requirements.
Your provider model must support state-specific roles, permissions, and documentation expectations, not one generic “provider.”
Why Fragmentation Has to Live in Config, Not Code
Hard-coding state rules (if state == ‘CA’…) guarantees:
- Fragile rollouts when laws change
- Divergent behavior in cloned features
- Hidden regulatory logic scattered across services
The only sustainable path: keep variability in a rules layer, not in business logic.
If you want to compare clinical cannabis workflows with the logistics-heavy world of last-mile fulfillment, the cannabis delivery app development guide offers a complementary look. It highlights operational constraints, compliance traps, and integration realities across state systems — useful context when designing a medical platform that must coexist with the retail layer.
Building for Multi-State Scalability Without Compliance Debt
Most teams don’t scale multi-state medical cannabis platforms—they accumulate conditional logic and pray regulators stop publishing PDFs. To survive State #7, #12, and #19, you need an architecture where new jurisdictions arrive as configuration and rules, not refactors.
The Real Anti-Pattern: State Logic Buried in Business Code
The universal failure mode:
- Launch in one state.
- Hard-code eligibility, limits, provider permissions, registry quirks.
- Expand, bolt on exceptions.
- Repeat until workflows behave differently across adjacent zip codes.
Scatter state logic across services and every expansion becomes a mini-refactor.
State-Specific Rules Engine: One Codebase, Many Personalities
Replace state-specific forks with a rules engine where policy lives in configuration:
1. Static Configuration
Eligibility criteria, registry fields, provider capabilities, reporting and retention.
2. Evaluated Rules
“Can this provider act here?” “Does this patient meet criteria?” “Is this product/dose allowed?”
3. Workflow Guards
UI/API gating and contextual errors.
One codebase, many regulatory personalities—no clones.
Configurable Compliance Workflows (Without Rebuilding Each State)
Onboarding, recommendations, refills, renewals, AE review all share one backbone. States only vary:
- Required vs optional steps
- Role permissions
- Required data
- Validity windows
You’re parameterizing a single workflow, not rebuilding ten.
Audit-Ready Logging as a Built-In Primitive
Audit logging must be:
- Event-complete (registrations → AE events)
- Immutable & queryable
- State-aware (“show all actions under State X”)
- Version-aware
If you can’t reconstruct what happened and why, you don’t have compliance.
Privacy-by-Design for Multi-State Care
Adding states shouldn’t require rebuilding PHI boundaries. Architecture must enforce:
- PHI vs non-PHI segregation
- Tenant isolation
- Scoped consent
- Logged, state-aware sharing
- Breach routing aligned to jurisdiction rules
Integration Abstraction: METRC and Its Successors Behind a Single Contract
Tracking systems will change—METRC today, something else tomorrow. Avoid bespoke integrations:
- Expose one internal contract for inventory, transfers, reconciliation
- Implement METRC, BioTrack, CCATS as adapters
- Keep mapping logic at the edges
Switching systems should be an adapter swap, not an architectural event.
Regulatory Change Management as a Product Feature
Design for constant legal churn:
- Versioned compliance matrices
- Versioned rules configurations with staging
- Go-live toggles for switching rule sets
- Impact simulations
- Visibility tools showing affected workflows
Early Wins That Prevent Long-Term Compliance Debt
Foundations that matter:
- Write the compliance matrix before code
- Loop compliance counsel into architecture
- Assume 12–18 months of volatility: use versioned configs and feature flags from day one
Treat multi-state scaling as a rules-and-configuration problem and your architecture stops being the bottleneck.
How Specode Helps Medical Cannabis Operators
You’re not building a nicer dispensary menu. You’re managing N-of-1 dosing, coordinating providers, and surviving multi-state compliance. Specode gives you the rails for that—and lets you own the train.
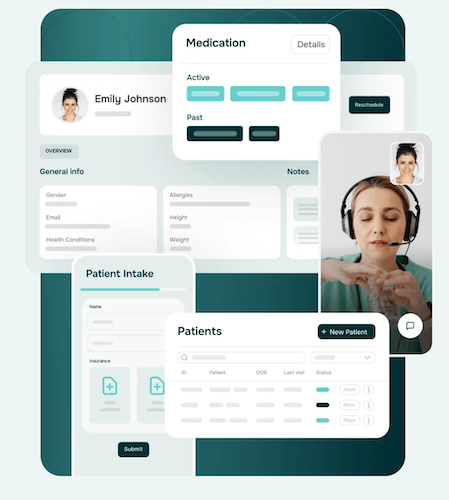
Specode as a Healthcare-Grade Foundation, Not a Vertical Toy
Specode works as a medical cannabis app builder the same way it works for RPM or chronic care: an automated platform with reusable healthcare components, a HIPAA-ready foundation, and an EMR-style data model instead of a shopping-cart schema.
Out of the box, you assemble on top of:
- Patient Dashboard & Profiles — condition-aware intake, history, symptom tracking
- Provider Profiles & Credentialing — license metadata, jurisdictions, state-ready role hooks
- Secure Telehealth & Messaging — async consults tied to recommendations and plan updates
- Basic EMR & Tracking Primitives — dosage logs, AE timelines, audit trails
- Scheduling & Consultation — indication/role-based booking wired to intake and plans
- Notifications & Check-Ins — route-aware reminders and outcome prompts
- Compliance & Audit Logging — immutable event logs from day one
The result: patient and provider dashboards that behave like clinical tools, not themed e-commerce.
Build Fast With AI, Without Handcuffing Yourself
Specode’s AI builder handles 0→1: screens, data models, workflow scaffolding for onboarding, dosing, and follow-up.
You can:
- Ship a HIPAA-ready MVP in weeks (often 4–6)
- Iterate via small prompts instead of multi-page specs
- Treat the AI-generated app like real code—extend and integrate as your protocols mature
Multi-State Without Cloning Your App Per Jurisdiction
Specode’s workflow and component model extends cleanly into a state-specific rules engine:
- Use configs for eligibility checks, documentation requirements, approval steps
- Run configurable compliance workflows—one onboarding skeleton, many personalities
- Leverage a state-aware logging and data model built for regulatory change management
Specode expects fragmentation; it doesn’t collapse when you add State #3.
Integrations on Your Terms
Because you own the code, integrations live in your app:
- Build adapters for METRC, CCATS, or other tracking systems
- Keep your cannabis EMR abstractions stable while swapping state systems
- Extend credential checks, registry sync, and reporting as rules tighten
Specode delivers the HIPAA compliant app framework and integration patterns; your team wires in the required stack—without waiting for a vendor roadmap.
The Real Trade: Compliance Plumbing vs Outcome Science
Specode doesn’t define THC/CBD trajectories or write protocols—that’s your edge.
It removes the expensive prerequisites:
- No blank-file dashboard design
- No reinventing audit-ready logging, consent, or PHI boundaries
- No replatforming when states or registries shift
You focus on outcome science and provider education. Specode handles the compliance scaffolding that keeps regulators calm and your roadmap intact.
Frequently asked questions
Because dispensary stacks are built for inventory and retail compliance, not clinical intake, dosing titration, PROs, adverse-event tracking, or state-aware provider credentialing.
Products vary, THC/CBD ratios shift per condition, and patients follow different trajectories. Without structured data, PROs, and a dosing engine, you’re guessing at scale.
If you store diagnoses, treatment decisions, or longitudinal outcomes—or exchange data with clinicians—you’re already operating at HIPAA expectations whether regulators say so or not.
Because state rules get hard-coded. Eligibility, registry steps, roles, documentation requirements, and reporting windows must live in configuration, not in intertwined business logic.
They can run a consistent 10–15 minute protocol—intake → risk review → recommendation → follow-up—without improvising or relying on personal notes outside the system.
Track outcomes. Platforms with structured PRO loops, clinician oversight, and timely dose adjustments dramatically outperform “unstructured use,” which has massive early drop-off.









