Digital Therapeutics (DTx) App Development Guide
Digital therapeutics app development isn’t just another branch of digital health—it’s where software starts behaving like medicine. The stakes are higher, the evidence bar steeper, and the rewards more tangible: reimbursement, prescription status, and integration into care pathways. But anyone who’s dipped a toe into this world knows it’s less “move fast and break things” and more “prove it, document it, and withstand an audit.”
That’s because digital therapeutics live under the same regulatory spotlight as medical devices. You’re not just designing screens and flows—you’re engineering outcomes, trial endpoints, and data pipelines that hold up to FDA and payer scrutiny. The upside? Products that actually change care delivery, improve adherence, and command real budgets.
If you’re serious about building software that treats conditions—not just tracks them—this guide walks you through the evidence, compliance, integration, and cost realities shaping DTx in 2025.
Key Takeaways
- Success in DTx hinges as much on operations and design as on algorithms. Evidence generation, FDA pathways, and interoperability with EHRs or medical devices often dictate adoption speed and reimbursement more than the therapeutic content itself.
- Creating digital therapeutics solutions isn’t about shipping another wellness app—it’s about proving measurable clinical outcomes with trial-grade evidence. From PHQ-9 score reductions to cost-savings data, payers and regulators only buy proof, not promises.
- The fastest, safest route to market in 2025 is assembling on HIPAA-ready rails with a healthcare AI builder, i.e., a digital health app builder that helps you reuse compliant components and ship faster. Specode lets you reuse compliant components, customize the last 20%, and keep full code ownership—cutting time and cost without boxing your DTx roadmap into a platform corner.
Is Digital Therapeutics (DTx) App Development the Right Path for Your Product?
Before committing to the long haul of DTx app development and design, it’s worth asking a blunt question: will your product clear the hurdles that separate wellness from medicine?
Unlike generic therapeutic apps, DTx must be built on clinical evidence and validated through clinical trials to prove clinical efficacy and meaningful health outcomes. That means your roadmap can’t skip the steps that lead to regulatory approval—and with it, market trust.
If your concept aligns with accepted therapeutic interventions—whether in behavioral health, chronic disease, or cognitive behavioral therapy—and you can commit to evidence based design, regulatory compliance, and measurable patient outcomes, the DTx path opens doors that wellness apps can’t:
- payer reimbursement
- prescribable status
- integration into standard care pathways used by healthcare providers
From prescription digital therapeutics for opioid use disorder to remote monitoring adjuncts in oncology, the field rewards products that prioritize patient engagement, treatment adherence, and strong clinical validation.
In return, the data—both trial-generated and real world evidence—can drive adoption at the provider, payer, and even policy level.
What Are Digital Therapeutics (DTx) — and How They Differ from Digital Health Apps
Here’s the short version: a digital therapeutics application is software that delivers a measurable, disease-targeted intervention—and has the receipts to prove it.

“Digital health” is everything else: tracking, education, coaching, content. Both can look like apps. Only one is expected to behave like medicine.
Plain-English Definitions
- Digital therapeutics (DTx): Software delivering an intervention intended to treat, manage, or prevent a condition. Think endpoints, protocols, and oversight.
- Digital health apps: Wellness helpers—useful, but not claiming to treat disease.
DTx vs. Wellness
- Claims: DTx can claim to treat/mitigate a condition (if supported). Wellness stays with “supports,” “encourages,” “helps track.”
- Proof: DTx lives or dies by evidence—study design, endpoints, durability—not vibes.
- Oversight: DTx is regulated as SaMD; wellness usually isn’t.
- Workflow fit: DTx must earn a spot in care pathways used by healthcare providers, not just the App Store.
Prescription vs. Non-Rx
- Rx DTx: Prescribed, labeled, often reimbursed. Distribution flows through clinicians and payers.
- Non-Rx DTx: Sold directly, but must be fanatically careful with claims (and usually won’t be reimbursed).
What you Can (and Can’t) Say
- If you treat anxiety, you need evidence tied to a clinical endpoint.
- If you support sleep hygiene, you’re likely in wellness—choose verbs wisely. Regulators read verbs the way lawyers read footnotes.
The Product Reality
Your DTx mobile app is just the patient-facing surface. Underneath sits the service: protocols, data services, audits, and often a clinician console. Regulators will judge you as digital therapeutics software, not a content site with notifications.
The North Star
If you want to build a digital therapeutics app, anchor everything to proof and labeling strategy first—claims, endpoints, and risk controls—then ship features that reinforce that contract with patients and clinicians. That’s how you earn trust, budget, and adoption.
Not legal advice. Talk to your regulatory counsel before you put a claim anywhere except the trash.
Benefits and Measurable Outcomes of Digital Therapeutics Apps
Short version: If you want to create a DTx app that earns a seat at the clinical table, it has to move hard clinical endpoints, keep people actively engaged in the therapeutic program long enough to matter, and show budget impact that a CFO can love.

(For clarity, we’ll reference standard clinical measures like PHQ-9 for depression, GAD-7 for anxiety, and ISI for insomnia when citing trial results.)
Clinical Impact (beyond “feels better”)
- Depression/anxiety (blended care): An 8-week “digital clinic” model cut Patient Health Questionnaire scores (PHQ-9) from ~13.4 to ~7.8 and Generalized Anxiety Disorder scores (GAD-7) from ~12.9 to ~7.4, with large effect sizes (d≈1.11 and d≈1.22). Completion rates hovered around 83%.
- Insomnia (digital Cognitive Behavioral Therapy for Insomnia, dCBT-I): Pivotal trials report over 60% remission (ISI<8) with a Number Needed to Treat (NNT) of ~2. Real-world cohorts mirrored these results—a rare case where everyday use matches randomized controlled trial (RCT) outcomes.
- Substance/opioid use disorder (SUD/OUD, adjunctive prescription digital therapeutics): Both RCTs and real-world studies show improved abstinence and treatment retention, especially when used alongside standard care (“adjunctive” approach).
Engagement and Adherence (the outcome multiplier)
- Human-in-the-loop models outperform “set-and-forget” software. In programs with provider or coach check-ins between visits, retention reached ~77–83% over active treatment periods and correlated with stronger symptom reduction. By contrast, a self-guided opioid use disorder PDT saw ~91% of patients disengage by week 12.
Economic Value (what payers actually buy)
- Healthcare resource use: For SUD, a pre/post claims study showed 56% fewer inpatient stays, 45% fewer ER visits, and ~$3,600 per-patient savings in six months.
- Cost-effectiveness: A 2024 review found DTx across multiple conditions to be cost-effective. The new ICER-PHTI framework places extra weight on near-term budget impact, meaning your evidence plan should target 12–24-month savings, not just lifetime quality-adjusted life years (QALYs).
RCT vs. Real-World Evidence (RWE): where it matters most
- When they match: Insomnia PDTs deliver comparable remission rates and NNTs in both trial and real-world settings—ideal for generalizability narratives.
- When they don’t: OUD outcomes can drop sharply outside trials without proper support infrastructure. In those cases, operational design—not the algorithm—is the limiting factor.
What This Means for Your Roadmap
- Design for proof, not just usage.
- Make engagement a feature of care, not a metric.
- Lead with budget impact.
DTx Taxonomy and Types of Digital Therapeutics Applications
When you think about how to develop a digital therapeutics app, the first strategic fork is deciding what kind of DTx you’re actually building. The taxonomy isn’t just academic—it determines your evidence burden, regulatory path, and ultimately whether payers will ever reimburse you.

By Prescription Status
- Prescription digital therapeutics (PDTs): FDA-authorized software, like EndeavorRx (ADHD) or RelieVRx (chronic pain). These require rigorous trials, physician prescribing, and face steep reimbursement hurdles.
- Non-prescription DTx: Direct-to-consumer or payer/employer distributed apps such as Omada or Noom. Evidence expectations vary, but they can scale faster by sidestepping prescriber bottlenecks.
Related: How to Develop an e-prescription App
By Therapeutic Modality
- CBT-based (DaylightRx for anxiety, Somryst for insomnia): evidence-heavy, relatively low build cost.
- Neurocognitive/gaming (EndeavorRx for ADHD): differentiated, but requires novel endpoints.
- VR/AR immersive (RelieVRx for chronic low back pain): high engagement, but device overhead.
- Biofeedback/monitoring (Propeller for asthma/COPD): strong adherence data, but integration with devices adds complexity.
- Coaching + protocols (Virta, Omada): scalable with human touch, payer-friendly .
By Role in Therapy
- Monotherapy DTx: Standalone interventions (RelieVRx, DaylightRx).
- Adjunctive DTx: Combined with drugs/devices (Rejoyn with antidepressants, Propeller with inhalers). Adjunctive often accelerates adoption because it extends existing care, rather than replacing it .
By Care Stage
- Prevention: Omada Prevent (prediabetes), Noom (weight management).
- Treatment: EndeavorRx for ADHD, Rejoyn for major depressive disorder.
- Maintenance: Propeller for COPD, Dario for diabetes monitoring.
Strategic Implications
- High-acuity conditions (e.g., PTSD, schizophrenia) demand deeper safety packages and longer timelines, but can command premium positioning.
- Employer and payer channels reward prevention and maintenance apps with faster adoption cycles.
- Modality drives engagement (VR can wow), but doesn’t guarantee superior outcomes—CBT-based apps often achieve comparable efficacy at lower cost .
Regulatory Pathways for DTx Apps
Here’s the reality check: no matter how slick your UX or how compelling your outcomes, regulators don’t buy vibes. They buy frameworks, filings, and claims that match the evidence behind your therapeutic intervention.

The SaMD Umbrella
Digital therapeutics are regulated as Software as a Medical Device (SaMD). That means the same rules that govern pacemaker firmware or imaging AI apply to your anxiety app if you’re making treatment claims. The burden shifts depending on risk: low-risk products may get enforcement discretion; higher-risk ones need a full dossier.
US FDA Pathways
- 510(k): If your app is substantially equivalent to a predicate (rare in DTx), this is the fastest path.
- De Novo: For novel, low-to-moderate risk DTx without a predicate. This has become the workhorse route for many first-to-market products.
- PMA (Premarket Approval): Reserved for high-risk products (Class III). Think seizure detection, schizophrenia adjuncts—heavyweight filings with pivotal trial evidence.
Pro tip: Pre-sub meetings (Q-Sub program) with the FDA are invaluable. Teams that engage early tend to cut months off timelines and avoid dead-on-arrival claims language.
Enforcement Discretion and Claims
The FDA occasionally exercises discretion (e.g., mental health apps during the COVID-19 PHE). But discretion isn’t strategy—count on it expiring. Labeling is your currency: what you can and cannot claim is defined as much by your submission as by your evidence.
Not legal advice: always align with your regulatory counsel before staking claims or locking in a pathway.
Clinical Validation Roadmap for Creating Digital Therapeutics Solutions
If you plan to develop DTx software, the clinical validation roadmap is where theory turns into credibility. Regulators, payers, and providers don’t care how sleek your app looks unless the evidence stands up to scrutiny.

Trial Design and Endpoints That Matter
Most digital therapeutics still rely on randomized controlled trials (67% of DTx studies today), but “sham app” controls or treatment-as-usual comparators are the norm—there’s no such thing as a sugar pill for software.
Increasingly, hybrid and adaptive designs are being adopted to cut timelines: think pragmatic trials run on patients’ own devices, or group-sequential designs that trim ~15% off sample sizes without sacrificing statistical rigor.
Endpoints and PROs (patient-reported outcomes) are under the microscope. Depression trials lean on PHQ-9, anxiety on GAD-7, insomnia on ISI. But digital biomarkers—like gait analysis from smartphones or heart-rate variability captured passively—are becoming legitimate alternatives.
FDA has already accepted digital endpoints in certain cases, and composite measures (clinical + engagement + usability) are emerging best practice for DTx.
From RCTs to Real-World Evidence
Real-world evidence (RWE) is now more than a post-market box-check. FDA is warming up to pragmatic trials embedded into care pathways, and 90% of U.S. payers demand robust trial data before coverage—even for post-market adoption.
Blue Cross plans already reimburse several prescription DTx, but only when RCT data is paired with economic modeling that shows clear cost offsets.
Case in point: Rejoyn (Otsuka/Click) for depression cleared FDA in 2024 on the back of a 386-patient sham-controlled RCT. Nerivio, a migraine device, proved its worth in a decentralized trial—patients recruited remotely, reporting a 2.7-day greater reduction in migraines than placebo. Both highlight the new playbook: agile trial design + validated endpoints + payer-ready health economics.
Finally, post-market doesn’t mean the finish line. Section 522 FDA authority can force ongoing surveillance, and payers increasingly tie reimbursement to outcomes-based contracts (adherence rates, symptom reduction, or even cost savings). Smart teams bake continuous evidence generation into their release plans from day one.
Core Product Capabilities in Building DTx Applications
A digital therapeutic succeeds when its core features serve both patients and clinicians—mapping directly to validated treatment plans while staying usable in day-to-day care.

Patient-Side Essentials
- Onboarding: Clear consent, safety, and data use.
- Therapeutic Scheduling: Daily CBT, sleep routines, dosing clarity.
- Content Modules: Structured interventions, adaptive lessons.
- Engagement Loops: Reminders, nudges, gamified streaks.
- Accessibility: Multilingual, screen-reader, low-literacy UX.
These aren’t extras—they’re the backbone of building DTx applications that patients can actually stick with.
Clinician-Side Capabilities
- Dashboards And Alerts: Highlight risk trends, not noise.
- Outcome Tracking: Show PHQ-9 drops, A1C trends, migraine-free days.
- Integration Hooks: EHR and claims workflows, or adoption stalls.
Bottom line: Cut the fluff, double down on features that prove adherence and outcomes—because that’s what payers, regulators, and clinicians are actually scoring you on.
Architecture and Data Flows
To make a digital therapeutics app that holds up under FDA review and payer scrutiny, the architecture has to be as rigorous as the clinical evidence. Most failures in this space aren’t about therapeutic efficacy—they happen because the underlying data flows weren’t designed like regulated medical software.

In fact, digital therapeutics platform development often succeeds or fails not on the therapeutic idea itself, but on whether the data plumbing is built to regulatory grade. Plumbing, not product-market fit, is where too many teams stumble.
Defining PHI Boundaries
Every DTx has to draw hard lines between what is PHI and what isn’t. Consent flows should make it crystal clear, and systems must enforce that boundary at the data model level. Metadata like “time of login” can become PHI fast when combined with clinical events—so you need schema discipline, not just legal disclaimers.
Auditability and Telemetry
An SaMD-grade system means every action is traceable. Who accessed what, when, and why needs to be logged in tamper-resistant trails that survive an auditor’s flashlight. On the flip side, telemetry streams (engagement data, sensor feeds, content completion) must be captured securely and segmented so ops teams can monitor performance without breaching PHI walls.
Release Governance
The real kicker: in DTx, shipping code isn’t “continuous delivery,” it’s controlled release. Each version needs lineage—what changed, how it was tested, and how it impacts clinical claims. FDA has already flagged ungoverned updates in software that altered dosing algorithms without documented impact analysis. Release governance is where QMS and dev velocity collide, and where too many startups learn the hard way.
Interoperability and Medical Device Integrations
If you’re asking how to create a digital therapeutics platform that doesn’t sit in a silo, interoperability is the make-or-break layer. The payoff: seamless data liquidity for patients, clinicians, and payers. The pitfalls: endless standards drift and brittle device integrations.
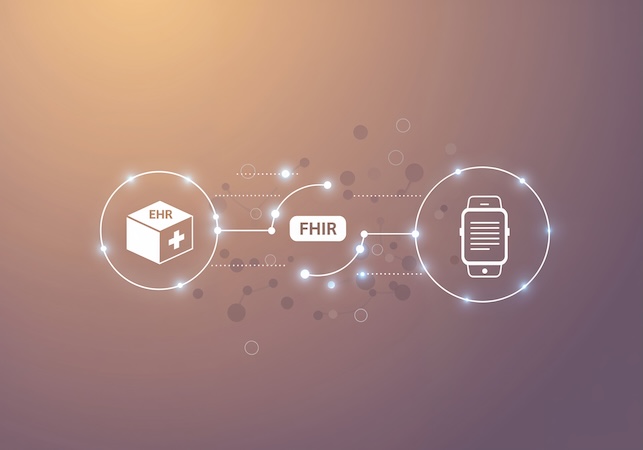
Connectivity priorities:
- FHIR/EHR Hooks: Most EHR vendors now support baseline FHIR APIs, but depth varies. Medication lists and scheduling are reliable; behavioral health and care plans often aren’t.
- RPM Device Data Pipelines: Blood glucose, spirometry, wearables—expect mismatched formats and spotty data fidelity. Device ingestion middleware (Mirth, Redox, Particle) often determines success more than the app itself.
- Formulary & Claims Feeds: For payer adoption, formulary status and claims integration trump nice-to-have features. This is where coverage decisions get automated.
- Enrollment vs. eRx: Many teams underestimate the gulf between patient self-enrollment and true e-prescribing. Getting into eRx flows requires certified intermediaries—budget both time and compliance overhead.
Using AI/ML to Create a DTx App Responsibly
AI is creeping into every corner of healthcare, and digital therapeutics are no exception. But the bar for “responsible” isn’t just model accuracy—it’s GMLP (Good Machine Learning Practice), bias monitoring, and the ability to prove your app doesn’t drift from its original claims.

- Bias & Monitoring: Models trained on narrow cohorts can underperform across demographics. Continuous monitoring—think real-world evidence feeds, not one-and-done validation—is essential.
- Change Control & Versioning: Every model update is a regulatory event. Without a clear paper trail, you risk invalidating prior clinical validation or triggering costly re-submissions.
- Evidence Impact: Payers and regulators will ask how evolving models affect outcomes. Documenting the impact on adherence, engagement, or clinical endpoints is non-negotiable.
Specode can build custom AI solutions tailored to your workflow, or plug in ready components like AI chatbots to enhance your therapeutic application.
Quality & Risk by Design in Therapeutics App Development
Digital therapeutics don’t get a free pass just because they live on a phone. The bar is the same as any regulated medical device: rigorous quality management, risk analysis, and end-to-end traceability. In practice, this means building quality and risk thinking into the product—not bolting it on before submission.

- Risk Management (ISO 14971): Identify hazards, estimate probability and severity, and design mitigations that hold up to auditor scrutiny.
- Software Lifecycle (IEC 62304): Treat your DTx codebase as SaMD, with defined development phases, verification checkpoints, and release documentation.
- Human Factors (IEC 62366): Usability is clinical safety—mis-taps or confusing flows can translate into adverse events.
- QMS & DHF (ISO 13485): Auditors expect a living design history file that connects requirements to risk controls, test results, and change logs.
For teams navigating digital therapeutics app development, these standards aren’t academic—they’re the practical guardrails that determine whether regulators, auditors, and hospital buyers trust your product. Verification and validation (V&V) close the loop: your app has to prove it works as intended, in the hands of real users, under real-world constraints.
Cost and Timeline Scenarios Creating a Digital Therapeutics Platform
The cost to how to create a digital therapeutics platform isn’t a single figure—it’s a function of evidence level, compliance scope, and integration demands. Think of it as three dials you can turn up or down depending on your strategy.
- Evidence: A lean pilot with feasibility data might run under $1M and wrap in 12–15 months. Pivotal RCTs with PROs and payer endpoints? Now you’re in the $5–10M range with timelines stretching to 3–5 years.
- Compliance: SaMD-grade risk management, 21 CFR Part 11 controls, and ISO-aligned QMS add both cost and time, but skipping them narrows reimbursement options and erodes payer trust.
- Integration: Plugging into EHRs, PBMs, or RPM pipelines can double the lift compared to standalone apps. Pear’s $1,300/course pricing vs. $136M annual spend is the cautionary tale here: integration costs that weren’t offset by scale.
The winning playbook in 2025 is milestone-based budgeting: fund feasibility, validate with real-world evidence, then scale reimbursement pilots. Some teams shave 30–40% of both development cost and timeline by assembling with reusable HIPAA-compliant components instead of coding from scratch—a Specode sweet spot.
How Specode Can Help Build a Digital Therapeutics App
Let’s be honest: most founders don’t need to reinvent regulatory compliance—they need to focus on clinical value. Specode accelerates that by shipping HIPAA-compliant components, rigorously designed for healthcare from Day 1. Think authentication, audit trails, secure data flows, plus telehealth, e-prescribing, care coordination, and more—all pre-tested and ready to go.
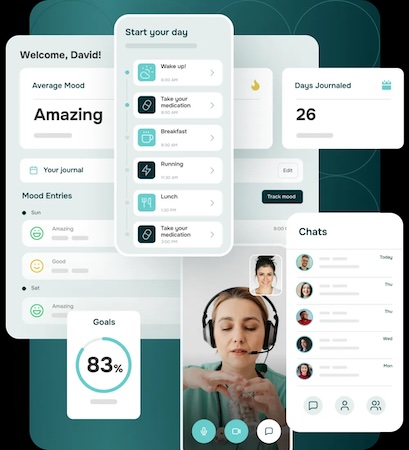
What this means for DTx teams:
- Reusable HIPAA-Compliant Rails: Authentication, data storage, PHI segregation, and release governance built in.
- Integration Flexibility: Canvas EHR supported out of the box; Epic, Cerner, and others handled via middleware or native APIs.
- Future-Proofing: Lab ordering, device sync, and eRx support available through partner integrations, not hacks.
Power of AI: Compose DTx by Conversation
Describe the flow—onboarding → eligibility → protocol assignment → session dosing → outcomes—and watch it take shape with an instant preview. Connect your own data early so the AI builder molds screens, schedules, and rules around your real content, cohorts, and measures (PHQ-9, GAD-7, sleep scores, etc.), not mockups.
Pair the assistant with your devs (or ours) when something’s truly novel—custom adherence logic, per-payer rules, or clinician dashboards—and spin up purpose-built AI agents on the Custom tier (e.g., coach/FAQ, ops helper). Fully brandable from day one. No AI magic—sequence and ruthless focus.
- Prompt → preview: tweak branching, dosing cadence, reminders, and paywalls in seconds.
- Integration switchboard: EHR/EMR, eRx, labs, wearables, payments/eligibility—stitched into your flows.
- Don’t rebuild what exists: modify packaged intake, journaling, scheduling, messaging; add only what’s net-new.
- Guardrails: Change Log restore and role-scoped testing keep iteration safe while you move fast.
- Your team or ours: combine AI-assisted assembly with custom development as needed.
You don’t just get a locked-down toy: you get 100% ownership of your codebase, full customization freedom, and the ability to extend or hand off the product later. Everything from your workflows to AI agents stays under your control—but built on a secure, composable foundation.
If your goal is to build your own DTx platform, Specode gives you head start, not handcuffs: fast, secure, and fully in your hands. Ready to see it in action?
Try Specode's AI builder free: make one small edit, see the preview, decide if it’s worth your next hour.
Frequently asked questions
Digital therapeutics are evidence-based, regulated software interventions designed to treat or manage a medical condition. Wellness apps may help with lifestyle changes but do not undergo clinical validation, cannot make medical claims, and are not subject to the same regulatory standards.
The timeline varies widely. A basic 510(k) pathway may take 12 to 18 months, while a full De Novo or PMA submission can stretch to 3 to 5 years depending on the complexity of the product and the supporting clinical data.
Typically, randomized controlled trials, pragmatic studies, or real-world evidence are needed to prove clinical efficacy. The level of evidence depends on the claims being made, but all must show measurable patient outcomes to satisfy regulators and payers.
Reimbursement can come through CPT or HCPCS codes, payer pilots, pharmacy benefit managers, or employer-sponsored programs. Coverage often depends on demonstrating both clinical effectiveness and cost savings.
In the United States, the FDA regulates DTx as Software as a Medical Device, most commonly through 510(k), De Novo, or PMA pathways. Each pathway depends on risk level, novelty of the device, and available predicate devices.









