How to Create a Remote Patient Monitoring Diabetes App
You’re not building an app; you’re standing up a 24/7 care loop that has to work at 3 a.m. when a CGM flirts with a low. In 2025, diabetes monitoring app development is about reliable data in, timely actions out, and audit trails that make your CFO smile.
This guide shows how to architect for real-time streams, keep alerts useful (not noisy), and prove value in the only metrics that matter: A1C, time-to-intervention, and avoided ER visits. We’ll cover native vs. cross-platform trade-offs, safe data pipelines, compliance you can actually ship, and a roadmap from pilot to scale. If you need something clinicians trust and payers fund, start here.
Key takeaways
- Operational excellence beats feature lists: normalize device data, separate safety vs. analytics paths, and tune alerts around Time-in-Range.
- Prove value early: track A1C deltas, time-to-intervention, and avoided ER visits—then align them to RPM billing.
- Build for scale on day one: HIPAA-by-design, partner-ready device adapters, and EHR-native workflows so pilots become programs.
The Rising Need for Remote Diabetes Monitoring
If your diabetes program still rides on quarterly A1C checks and a couple of fingersticks, you’re trying to win 2025 with a 1999 playbook. The burden has outgrown the clinic calendar.

If you’re exploring diabetes monitoring app development in 2025, here’s why the timing is now—not “sometime after the next procurement cycle.” The burden has outgrown the clinic calendar, and continuous data is finally useful for diabetes care.
- the scale problem
1 in 9 adults lives with diabetes today; IDF projects 1 in 8 (~853M) by 2050, with ~252M undiagnosed, a quiet pipeline of diabetes patients headed for avoidable diabetes complications.
- the cost problem
U.S. spend hit $412.9B in 2022 (direct + productivity). If you want CFO attention, that’s it—continuous, not episodic, care moves the needle on patient outcomes.
- the access problem
Nearly 70% of U.S. counties have no endocrinologists. And across 15 large metros, new-patient waits now average 31 days. Translation: reactive care by default unless you bring data in between visits with remote monitoring.
- the volatility problem
Glycemic risk doesn’t wait for appointments. Adults with diabetes average ~72 ED visits per 1,000 annually; hypoglycemia alone drives ~202k ED visits each year. Proactive hypoglycemia alerts and near-real-time coaching reduce those spikes before they become admissions.
- the data problem (ironically the opportunity)
Modern continuous glucose monitoring sensors stream up to 288 readings/day—finally enough clinical data to act on glucose levels in real time. That’s why teams are shifting day-to-day decisioning from pure A1C levels to Time-in-Range—an operational health metrics play that requires real-time monitoring and smart triage.
Does Remote Monitoring Actually Move Outcomes?
Yes—consistently, if not magically. Recent syntheses show telehealth/RPM lowers A1C by ~0.3–0.5% on average, with CGM adoption itself delivering modest but significant A1C drops in type 2. That’s not just statistical: at population scale, a half-point reduction is fewer ER spikes, fewer admissions, and a healthier payer mix.
Bottom line. The curve (prevalence, costs) is going up; specialist supply and appointment access aren’t. Meanwhile, patient data from wearable devices and connected medical sensors is continuous.
The only defensible operating model is always-on: stream blood glucose from the glucose monitoring devices into a diabetes monitoring application, triage with data analytics, intervene early, and document outcomes.
Market Outlook and Business Case
If you’re exploring diabetes management app development, the market timing has rarely been better. Two strong tailwinds—a booming device layer and stable reimbursement frameworks—are making it easier to turn an idea into a viable remote patient monitoring system.

RPM Market Growth (Diabetes Tailwinds)
- CGM goes mainstream. FDA cleared the first OTC continuous glucose monitors in 2024—Dexcom Stelo and Abbott Libre Rio/Lingo—expanding access beyond insulin users. This widens the addressable base for any diabetes management platform and strengthens the case for integrated glucose monitoring app capabilities.
- Utilization is climbing in public programs. ADA’s 2025 access report confirms that type 2 usage, which first surpassed type 1 back in 2022, has continued to accelerate through 2024. More patients using connected medical devices means software teams can design for population-scale patient engagement rather than niche pilots.
- Policy stability helps planning. CMS’ April 2025 guidance keeps telehealth flexibilities through September 2025 and reiterates RPM rules, giving developers and healthcare providers a predictable environment for scaling chronic disease management solutions.
ROI For Providers, Payers, And Startups
- Clinical effect (the lever): Well-designed diabetes RPM programs consistently show modest but real A1C drops (~0.3–0.6%). This can improve treatment adherence, boost patient compliance, and reduce acute episodes that often lead to costly admissions.
- Economics (the justification): A 2025 cost-utility analysis found real-time CGM to be cost-effective versus SMBG from a Medicare perspective, especially when integrated into workflows that include care coordination and timely medication reminders.
- Operator take: By connecting blood sugar tracking app data with outreach workflows—possibly enhanced by carbohydrate tracking and insulin dosage logging—providers can turn continuous data into actionable interventions without overloading staff.
Insurance Reimbursement Pathways (U.S., Medicare)
- RPM (device-agnostic) codes:
- 99453 – setup/education (once)
- 99454 – device supply/data transmission (≥16 days/30-day period)
- 99457 – first 20 min treatment management (interactive)
- 99458 – each additional 20 min
- 99091 – data collection/interpretation
These are the operational backbone for most reimbursable telehealth integration strategies. For telemedicine app development, wire visit scheduling, consent capture, and time tracking into the same workflows that log RPM minutes, so virtual visits, messaging, and documentation roll up cleanly to billing.
- CGM-specific professional services: 95249/95250 (sensor initiation/training) and 95251 (analysis/reporting) are common in hybrid RPM + in-clinic models.
- Compliance and infrastructure: Success isn’t just billing—it’s building for HIPAA compliance, FDA regulations, and end-to-end data security with proper encryption, plus future-proofing for bluetooth connectivity and cloud storage so device data flows seamlessly into your platform.
One-line business case: A strong diabetes management platform that links continuous data from connected medical devices with proactive care workflows not only delivers measurable clinical impact—it’s also reimbursable today, making it a sustainable play for startups and established providers alike.
Types of Diabetes Monitoring Apps
Not all diabetes software is created equal. When you set out to create diabetes monitoring app experiences that actually move outcomes, it’s worth knowing the three main categories and how they fit into modern care models.

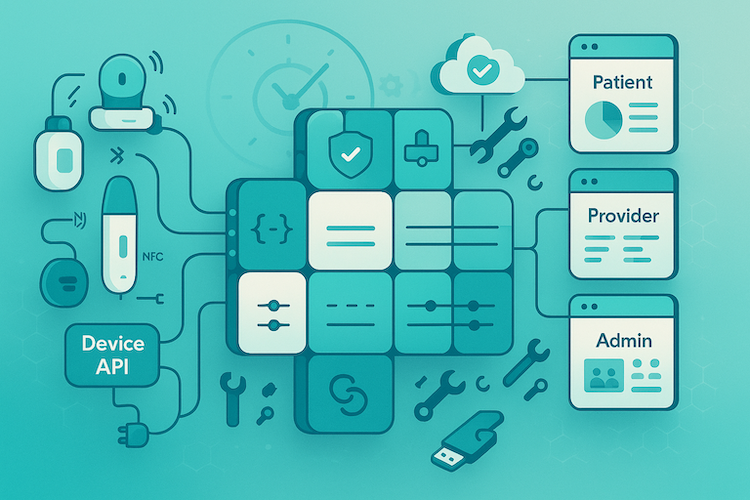
Patient-Centric Apps (Self-Management)
This is where patients live day-to-day: apps designed to support their diabetes care and make the routine feel manageable. A well-built patient app often includes:
- Real-time glucose visualization via CGM or manual entries
- Insulin management tools for tracking doses, timing, and delivery methods
- Medication reminders and carbohydrate tracking to build adherence habits
- Trend insights that highlight stability or variability without overwhelming the user
- Engagement features such as progress milestones, health streaks, or quick coach check-ins
Why it matters: When patients feel in control and supported, you get better treatment adherence, reduced emergency events, and stronger patient compliance. These apps form the foundation of long-term chronic disease management.
Provider Dashboards (Population Health & Clinical Decision Support)
On the other side of the data stream are the clinicians, care coordinators, and administrators who need actionable visibility across diabetes patients.
Key elements include:
- Population-level overviews with aggregated health metrics and risk flags
- Alerts and decision support for patients trending toward hypo- or hyperglycemia
- Care coordination tools to assign follow-up tasks and document interventions
- Integration with EHR systems and other clinical platforms for a complete picture
- Analytics dashboards to track outcomes, optimize workflows, and justify investment to stakeholders
Why it matters: These tools turn raw CGM or blood sugar tracking app data into targeted actions for healthcare providers, enabling proactive interventions instead of reactive crisis management.
Hybrid Platforms (RPM + Telehealth + Coaching)
Hybrid platforms combine the best of both worlds: patient self-management and provider oversight. They typically feature:
- Continuous data flow from connected medical sensors into both patient and provider interfaces
- Telehealth integration for virtual visits triggered by real-time risk patterns
- Coaching overlays—human or automated—offering guidance based on insulin management trends, carbohydrate logs, or missed medication reminders
Why it matters: This model allows timely interventions, personalized care plans, and scalable operations. It also aligns closely with reimbursement pathways that reward remote patient monitoring system deployments paired with telehealth integration.
Specode’s take: Whether your goal is to create diabetes monitoring app for self-management, equip clinicians with dashboards, or launch a hybrid RPM + coaching platform, Specode’s reusable HIPAA-compliant modules speed up the build. From insulin management components to secure device integrations, you can go to market faster without cutting clinical or regulatory corners.
Core Features That Make or Break a Diabetes RPM App
If you’re figuring out how to create a diabetes app that earns clinician trust, keeps patients engaged, and satisfies administrators, it’s not just about ticking feature boxes. It’s about building each capability to meet clinical-grade standards and regulatory expectations from day one.

Patient-Facing
These features need to go beyond “nice to have” — they should actively shape patient behavior and improve safety:
- Real-time glucose tracking: Pull continuous data from CGMs and fingerstick glucometers with low latency, so patients can respond to trends before they become emergencies.
- Medication reminders: Automate nudges based on prescription schedules, time-in-range performance, or pattern recognition in missed doses.
- Diet, activity, and carb logging: Integrate manual and sensor-based inputs (e.g., step count, nutrition scans) to help patients see the link between lifestyle and glycemic variability.
- Hypo/hyperglycemia alerts: Configure threshold-based alerts that escalate to caregivers or care teams if the patient doesn’t respond.
- Accessibility features: Incorporate voice controls, high-contrast themes, larger tap targets, and haptic feedback for users with vision impairment or neuropathy.
Provider-Facing
Provider tools should make high-volume patient oversight efficient and clinically meaningful:
- Continuous data streams from CGMs & glucometers: Deliver device-agnostic, normalized feeds into one interface, so clinicians aren’t juggling multiple portals.
- Population analytics & risk stratification: Identify high-risk cohorts automatically, highlighting patients with rapid A1C deterioration or repeated hypo/hyper episodes.
- EHR integration & clinical notes: Support bi-directional sync with leading EHRs so that every glucose reading, intervention, and follow-up task is part of the official patient record.
Administrator-Facing
Admins care about compliance, efficiency, and measurable performance:
- Billing & reimbursement support: Build workflows that map directly to CPT/HCPCS codes for RPM, telehealth, and CGM services — with automated documentation to meet audit requirements.
- User management: Control access by role (patient, provider, admin, coach) with full HIPAA-compliant authentication and activity logging.
- KPI dashboards: Track clinical outcomes, patient engagement rates, and reimbursement capture in one place to guide operational decisions and prove ROI.
Specode’s angle: Our reusable components handle the heavy lifting for all three user types, from secure device integration to analytics pipelines, so teams can focus on the parts of how to create a diabetes app that differentiates their brand — not the plumbing.
Integration with Devices and Wearables
You don’t win this category with “yet another dashboard.” You win it by nailing device plumbing on day one—clean data in, low-latency signals out, and zero drama for clinicians. If your mandate is to develop diabetes monitoring application workflows that scale, start here.

CGMs, Smart Pens, Fitness Trackers — What actually ships data
CGMs (the data engine)
- Dexcom G7 now supports direct-to-Apple Watch (no phone relay) via Bluetooth—fewer failure points for patients who live on their wrist.
- Abbott FreeStyle Libre 3/3 Plus streams real-time glucose to the phone; Abbott’s OTC line (Libre Rio/Lingo) broadens non-insulin and wellness use cases.
- Medtronic: MiniMed 780G currently pairs with Guardian 4; Simplera Sync CGM received FDA approval with a U.S. limited launch slated fall 2025.
Smart Insulin Pens (closing the loop without a pump)
- Medtronic InPen pushes dose data via Bluetooth into its app and supports CGM integrations.
- NovoPen 6 / Echo Plus transfer dose history to apps like Glooko via NFC tap.
- Bigfoot Unity layers smart pen caps on Abbott Libre 2 data for real-time dosing guidance; Abbott completed the Bigfoot acquisition in 2023.
Activity/Fitness Signals (context, not diagnosis)
Apple HealthKit / Android Health Connect expose blood glucose and activity data types, so you can correlate steps/sleep with glycemic variability. Note: Dexcom’s Android sharing to Health Connect carries a 3-hour delay—don’t key safety logic off third-party mirrors.
Brand Ecosystems and API Realities
- Dexcom: Mature Developer Program with a documented Web API (REST) for authorized partners; production access requires approval. Pair this with Dexcom Clarity for clinician reporting.
- Abbott: Clinical cloud is LibreView; official partner integrations exist (e.g., NovoPen 6/Echo Plus). Public API docs aren’t broadly open—expect partner onboarding or indirect access via authorized aggregators.
- Medtronic: Clinical cloud is CareLink. Public, production-grade APIs aren’t openly advertised; integrations are typically via Medtronic partnerships or patient-mediated exports (community reverse-engineering exists but isn’t appropriate for regulated products).
Exec takeaway: Plan on multi-path ingestion—direct vendor APIs where available (Dexcom), partner programs or clinical clouds (LibreView/CareLink), plus HealthKit/Health Connect for lifestyle context. Your legal and QA teams will thank you later.
Treat medical device integration as a product capability, not a one-off project: define a vendor-agnostic schema, isolate adapters behind stable interfaces, and make swap-outs low risk for clinical ops.
Transport Choices: Bluetooth, NFC, and Cloud Sync
- Bluetooth (BLE): Your default for continuous streams (Dexcom G7 → phone/watch; Libre 3 → phone). Lowest latency for alerts; power and pairing UX matter.
- NFC: Great for tap-to-transfer dose history from smart pens (NovoPen 6/Echo Plus) and for certain Libre workflows; low battery cost, but not a live telemetry channel.
- Cloud sync: Each vendor runs its own clinical cloud—Dexcom Clarity, Abbott LibreView, Medtronic CareLink—which you’ll likely integrate for longitudinal reporting and sharing with HCPs. Design your pipelines so device → app (BLE) handles real-time safety, while cloud → EHR handles audit-ready history.
Build Decisions That Keep You Out of Trouble
- Normalize early. Unify CGM payloads into a common schema before analytics; vendor quirks multiply at scale.
- Separate safety from convenience. Use first-party BLE streams for hypoglycemia logic; treat aggregators/Health Connect as enrichment only (remember the Android 3-hour delay).
- Design for offline. Queue readings and alerts locally; reconcile to cloud when connectivity returns.
- Credential the ecosystem. Expect partner reviews (especially for Dexcom full access) and document your security posture for HIPAA and vendor audits.
- Prove the round-trip. For every device: demonstrate device → app → cloud → EHR → clinician action → patient outcome, not just “data lands somewhere.”
If you want this operational without 6 months of yak-shaving, we can map your device list to concrete ingestion paths (API vs. partner vs. patient-mediated), then slot Specode’s connectors for the first sprint.
Compliance and Regulatory Framework
Short version: compliance is the product. If you’re building diabetes tracking app workflows that touch PHI and steer care, design HIPAA, FDA, and security into the architecture—not into a binder after kickoff.

HIPAA and Patient Data Rights
HIPAA’s Security Rule expects risk-based controls: treat “addressable” encryption as mandatory, implement real audit controls, and honor the Right of Access (deliver electronic records in the requested format within 30 days). Build breach response like you’ll need it: detect, assess, and notify (individuals + HHS) within 60 days.
- Ship export/fulfillment flows in the product, not as a help-desk promise.
- Make audit logs tamper-evident and time-synced across services.
FDA Lines and Near-Term Changes
If your software merely supports a clinician and they can independently review the basis, you’re likely Non-Device CDS. The moment you drive diagnosis/treatment—or hide the rationale—you’re a medical device (think 510(k)/De Novo) and need a QMS.
FDA’s QMSR aligning Part 820 to ISO 13485 lands Feb 2, 2026; the 2025 cybersecurity guidance expects secure design, SBOMs, and threat modeling in submissions. Decide early which side you’re on and staff accordingly.
Security Baselines That Pass Procurement
Encrypt in transit (TLS 1.3 preferred) and at rest with proper key management; protect mobile caches/logs; prove accountability with immutable access/admin/API/export logs; rehearse incident response.
- Crypto: TLS 1.3, modern ciphers, AES-grade at-rest encryption, key rotation.
- Logging: Immutable, retention-policy-backed, and queryable across tenants.
- Incident: Practiced runbook—detect → contain → notify within statutory clocks.
Executive takeaway: Bake HIPAA access, logging, and breach workflows into day one; choose your FDA path before scoping features; and hold engineering to NIST/HHS-aligned security so procurement and payers see a deployable product, not exceptions.
Architecture and Roadmap: Ship Your Diabetes RPM App Without Drama
This combined diabetes app development guide is the “how we’ll ship without drama” plan: the tech choices that won’t age poorly, plus a pragmatic path from zero → pilot → scale.
If you’re coming from healthcare app development, treat sensor streams as first-class citizens: design for offline, normalize early, and keep safety paths separate from analytics so alerts never wait on the data warehouse.

1. Architecture That Can Survive Real Patients
Mobile
- Rule of thumb: heavy BLE, background sensing, and watch support → go native (Swift/Kotlin). Provider/admin UIs with light device work → cross-platform (React Native/Flutter) is fine.
- Offline-first: queue readings/alerts locally, reconcile on reconnect. Kill flaky background tasks early.
- Safety split: run safety-critical logic (hypo alerts) off first-party streams; use third-party aggregators for enrichment only.
Backend
- Event-driven core: device→ingestion→queue (e.g., Pub/Sub/Kafka)→processors→stores.
- Stores with intent: time-series (glucose), relational (patients/orders), object (raw payloads), immutable audit log (append-only).
- Security by design: per-tenant keys, short-lived tokens, kms-managed secrets, least privilege, reproducible infra (IaC), SBOMs in CI/CD.
Interoperability and Device Middleware
- Normalize early: map vendor payloads into a common glucose schema before analytics.
- Healthcare plumbing: FHIR R4 for clinical resources, SMART on FHIR/OAuth2 for auth, HL7 v2 for legacy feeds; use middleware (e.g., Mirth, custom services) to bridge EHR quirks.
- Contracts: versioned APIs, schema evolution, and synthetic data generators for repeatable tests.
2. A Step-By-Step Build That Busy Teams Can Actually Run
1) Clinical Needs & Guardrails
Define who you will help and how you’ll prove it. Co-write safety boundaries with a clinician (what won’t the app do—e.g., no autonomous dosing).
Exit: one-page care model, key risks, success metrics, do/don’t list.
2) Requirements And Ruthless Prioritization
Turn the care model into epics: patient app, provider console, ingestion, analytics, compliance. Cut features that don’t move outcomes or reimbursement.
Exit: v1 scope, acceptance criteria, performance/SLA budgets.
3) UX for Diabetic Populations
Large touch targets, high-contrast modes, haptics/voice for neuropathy/vision issues. Design alerts with escalation paths, not just push spam.
Exit: click-through prototypes, empty-state content, edge-case flows (low battery, no sensor).
4) Device Integration and Test Harness
Stand up BLE/NFC wrappers, a synthetic CGM stream for CI, and a lab app that spoofs bad data (drift, gaps, duplicates).
Exit: green tests on: pairing, dropout recovery, clock skew, duplicate suppression, and alert latency.
5) Compliance and Security Bake-in
Wire audit logging, PHI tagging, export flows (Right of Access), and breach runbook triggers. Threat-model safety logic; encrypt in transit (TLS 1.3) and at rest with managed keys.
Exit: traceable logs, passing static/dynamic scans, documented risk decisions.
6) Pilot with Real Care Teams
Small cohort, daily huddles, alert fatigue tuning, and support runbooks. Measure “time-to-intervention” and false-positive rate, not just DAU.
Exit: post-pilot report, change list, go/no-go for scale.
7) Scale and Operate
Sharding/partitioning for time-series, autoscaling processors, SLOs for ingestion and alerting, and on-call rotations that won’t burn out your team.
Exit: capacity plan (x patients, y events/sec), cost envelope, and quarterly security/compliance drills.
3. Decision cheat-sheet
- Native vs cross-platform: pick native if you need rock-solid sensors/watch + background processing; else mix: native patient app + cross-platform provider UI.
- Data model: design a normalized glucose domain once; everything else hangs off it (alerts, analytics, billing).
- Interoperability: FHIR where possible, HL7 v2 where necessary, middleware where reality bites.
- Safety: separate “notify now” from “analyze later” paths—don’t make the pager wait for the data warehouse.
Monetization Models That Actually Scale Diabetes RPM
You’ve built the thing—now it has to pay for itself. In diabetes RPM, three revenue paths tend to dominate:

Subscription vs RPM Reimbursement
If you’re selling direct to consumers, subscription is straightforward—tiered plans for features, coaching, or bundled device shipments. But in the U.S., the real money is in RPM reimbursement. CPT codes 99453, 99454, 99457, and 99458 let providers bill for setup, device data, and ongoing monitoring time. That means your platform must track minutes, device usage, and outcomes cleanly enough to survive an audit.
Partnerships with Payers and Device Makers
Payers are incentivized to back RPM if you can show reduced admissions or ER visits; device makers want sticky software ecosystems. Strike co-marketing or data-integration deals where your app becomes the default dashboard, or bundle your service with CGM/pen hardware to lower acquisition costs for both sides.
3. White-Label Licensing
If brand-building isn’t your goal, license your platform to clinics, hospital systems, or even other startups. This model thrives if you’ve nailed compliance, device integration, and can offer turnkey deployment under someone else’s logo—bonus points if you’ve already aligned to their EHR and billing systems.
Bottom line: Pick the model that matches your buyer. If your end user is a patient—subscription works. If it’s a clinic—build for CPT billing. If it’s everyone—make your core product licensable. The business model is just another architecture decision, but it’s the one that decides whether you’re a pilot project or a line item in next year’s budget.
Challenges and How to Overcome Them
Short version: most diabetes RPM failures aren’t technical—they’re operational. Solve the ops, and the tech suddenly looks brilliant.

Device Interoperability Headaches
Different CGMs, partner-only APIs, and “coming soon” features turn roadmaps into spaghetti.
Fix: define a single glucose domain model and normalize every payload to it; treat vendor SDKs as replaceable adapters behind a thin interface. Build a synthetic CGM stream for CI so you can test dropout, drift, duplicates, and clock skew daily.
Separate safety paths (first-party BLE streams for alerts) from analytics paths (cloud/aggregators). Assume partner onboarding takes quarters, not weeks—design patient-mediated fallbacks (e.g., HealthKit) for enrichment, not safety.
User Adoption and Engagement Drop-off
The #1 killer is friction: pairing hiccups + alert fatigue = churn.
Fix: make Day-1/7/30 activation a product metric with owners; implement one-tap recovery for pairing, and preempt alert fatigue with rate-of-change logic, quiet hours, and escalation paths (push → SMS → human).
Tie nudges to Time-in-Range or concrete next steps (“scan sensor now,” “eat 15g carbs”), not generic cheerleading. Treat “missed logins” as a clinical signal—route to a coach, not a marketing drip.
Regulatory Delays
Partner reviews, IRB questions, and security audits can freeze momentum.
Fix: run parallel tracks from day one:
- a lean QMS-lite (requirements → V&V → traceability) that can expand to ISO 13485 if needed;
- a ready-to-send security due-diligence pack (architecture, data flows, SOC2/HIPAA mappings, pen-test summary);
- a regulatory decision tree—Non-Device CDS vs Device—so features don’t wander into 510(k) land by accident. If you might be a device later (dose logic), book a pre-sub early.
Data Overload for Providers
A thousand alarms that say “do something” equals nothing.
Fix: deliver ranked, batched work—not raw streams. Score risk with TIR + rate-of-change + recent events, and group alerts by patient/day. Make the inbox action-first (acknowledge, message, schedule, adjust plan) and document time automatically for reimbursement.
Measure time-to-intervention and false-positive rate weekly; if either drifts, tune the thresholds before adding “more AI.”
Operational Checklist (Clip-And-Ship):
- One normalized glucose schema; adapters per vendor; synthetic data in CI.
- Two data lanes: real-time safety vs batch analytics.
- Guardrails for Day-1/7/30 activation; alert rate limits + escalation.
- Reg path chosen early; QMS-lite + security pack ready.
- Provider inbox = ranked actions, not graphs; track TTI and FPR as SLAs.
Do this, and the four “hard problems” become regular maintenance instead of weekly fire drills.
Cost of Developing a Remote Patient Monitoring Diabetes App
Your budget is driven by devices, compliance, and proof. Features are cheap; integrations and validation aren’t.
Order-of-magnitude budget split (for a serious v1 → pilot):
- Device & EHR integrations: 25–40%
- HIPAA-by-design plumbing (auth, audit, exports, encryption, logging): 15–25%
- Patient + provider apps (UX, alerts, workflows): 20–30%
- Analytics & reporting (risk, TIR, reimbursement artifacts): 10–15%
- Clinical validation & security testing: 10–20%
Impact of Device Integrations
Each CGM/smart pen adds adapter work (BLE/NFC + cloud), partner onboarding, and long-tail maintenance. Plan test harnesses (synthetic CGM streams, dropout/drift scenarios) and multi-path ingestion (vendor API + patient-mediated sources) or you’ll pay in support later. Adding a second device brand typically costs less than the first—but still requires QA, docs, and ops playbooks.
Custom vs Reusable HIPAA-Compliant Components
Rolling your own auth, PHI tagging, audit trails, Right-of-Access exports, breach hooks, and key management is months of engineering plus ongoing audits. Reusing hardened components usually saves 30–50% of build time and cuts compliance risk because controls are consistent across services. You still own UX and clinical workflows—the parts that differentiate you.
Clinical Validation Costs
Two lanes:
- Non-Device CDS: pilot with real teams, measure A1C/TIR and time-to-intervention, tighten alerts, document outcomes. Expect spend on clinician time, IRB (if needed), analytics, and security due-diligence packs.
- Regulated device territory (dose calculators/control): add QMS, V&V, cybersecurity documentation, and (often) a pre-sub → 510(k)/De Novo path. Budget for specialist consulting and months of verification—this is where timelines expand.
Bottom line: Control costs by normalizing device data once, reusing HIPAA-grade plumbing, and picking your validation lane early so scope doesn’t drift into a regulatory rewrite.
Best Practices from Successful Implementations
What the winners do: They run human-in-the-loop care on top of frictionless devices and EHR-native ops. Tech isn’t the hero; it’s the force multiplier that routes scarce clinical time to the right patient, at the right moment.

Case Study Snapshots (signal, not fluff)
- DHRCP (clinic-led, high-touch): CDCES calls every 1–2 weeks with rapid med titration under endocrinology supervision; grads dropped A1C from 10.4% → 7.0% (~–3.4 points) in ~161 days. Clinical intensity works—just make it scalable with triage.
- Livongo + Harris Health (commercial, ROI-first): Cellular meter (zero pairing), unlimited strips, 24/7 coaching. $80 PMPM savings (Y1), $154 PMPM (Y2), 2.1× ROI (Y2), +92 NPS, and fewer hypoglycemic days (–21%).
- Ochsner Digital Medicine (health-system native): Tight EHR integration; licensed clinicians + coaches adjust meds “on the fly.” –15% hospital admissions, –41% ER visits; 81% hit A1C goal within 6 months.
- Omada + Essentia (engagement engine): Multi-channel enrollment (EMR prompts, incentives, internal social). >25% above enrollment targets; 76% hit A1C-reduction goals in year one.
KPIs That Actually Matter
- A1C improvements: Expect ~–0.55% as a conservative baseline; –1.15% to –3.4% with high-intensity models or high-risk cohorts. Tie your product bets to the clinical intensity you can sustainably deliver.
- Patient compliance/adherence: Top programs hit ~90% adherence. Targeted “adherence calls” lift transmission from 45.9% → 60.2% (non-adherent) and 82.8% → 91.1% (already adherent). Plan for 9–21% attrition unless you design against it.
- Readmissions / acute utilization: System wins are fewer admits/ER visits: –15% admissions and –41% ER at Ochsner; many orgs report admission/readmission drops when RPM is done right. Build an admin dashboard that proves this in CFO language (PMPM, avoided admits).
Copy-this playbook
- Triage-first clinician worklist (actionable, ranked; no raw stream surfing).
- Frictionless devices + supplies (cellular where possible; auto-replenish).
- EHR-native ops + billing capture (document time, close loops, show ROI).
How Specode Accelerates Diabetes RPM App Development
You don’t need another vendor; you need runway. Specode is an automated platform with reusable HIPAA-compliant components that lets your team ship the hard parts—secure data flows, device plumbing, audit-ready logging—without reinventing them.
Compose RPM with AI Builder by Chatting
Describe the flow—enroll → pair device → set thresholds → route alerts → document & bill—and watch it assemble with an instant preview. You start on healthcare rails (roles, consent, audit), so you’re shaping protocol logic, not rebuilding scaffolding.
Connect your own data early and the assistant molds screens and rules around real patients, providers, and metrics (e.g., time-in-range, A1c cadence).
- Prompt → preview: tweak alert thresholds, outreach cadences, patient messages, and note templates in seconds.
- Integration switchboard: CGMs & smart pens, labs (A1c), EHR/EMR (Canvas out-of-the-box; enterprise EHRs scoped case-by-case), pharmacy/supplies, eligibility & payments—stitched into your flows.
- Guardrails: Change Log restore and role-scoped testing keep iteration safe while you move fast.
- Your team or ours: combine AI-assisted assembly with your devs, or tap our Custom tier for managed help and purpose-built AI agents (e.g., pattern-aware coaching or ops assistants).
- Don’t rebuild what exists: modify packaged intake, scheduling, messaging; add only what’s net-new to your RPM program.
No AI magic—sequence and ruthless focus so you move from “first signal” to “clean claims” without losing runway.
Faster Device API Integration
We can quickly spin up ingestion, normalization, and alerting modules for CGMs and smart pens, with clean adapters so you can swap vendors without refactoring your core. (EHRs are case-by-case via middleware like Mirth or native APIs; Canvas Medical is supported out of the box.) Result: days to first signal, not months.
Built-in Compliance and Security
Encryption in transit/at rest, PHI tagging, immutable audit logs, right-of-access export flows, breach runbook hooks—wired from day one. Your security team gets artifacts, not promises.
Your Code, Your Cloud, Your Workflows
No lock-in. You own 100% of the code, deploy to your cloud, and customize almost everything—from risk scores and alert thresholds to note templates and billing capture—so it fits how your clinicians actually practice.
Illustrative Timeline (What “Fast” Looks Like):
- Weeks 0–2: Stand up auth, audit, data model; connect first CGM in a sandbox; synthetic streams in CI.
- Weeks 3–6: Patient app + provider console MVP; real device pairing.
- Weeks 7–10: Pilot with a small panel; tune thresholds and outreach; flip on reimbursement workflows.
- Post-pilot: Scale patients, harden SLOs, add second device brand/EHR lane.
If you want a pragmatic path from “prototype that demos well” to “program that bills cleanly,” let’s talk. We’ll show you live modules, map them to your stack, and co-design a two-sprint starter plan on how to build a diabetes management app.
Start free on Specode—begin assembling your remote patient monitoring diabetes app with the healthcare AI builder, then plug in real data and integrations when you’re ready.
Frequently asked questions
CGMs (e.g., Dexcom, Abbott Libre, Medtronic), Bluetooth glucometers, smart insulin pens (e.g., InPen, NovoPen 6/Echo Plus, Bigfoot Unity caps), and select insulin pumps can connect. Smartwatches and fitness trackers add context (activity/sleep). Data arrives via BLE/NFC and vendor clouds like Clarity, LibreView, or CareLink.
Continuous data enables earlier interventions, fewer hypo/hyper events, and steadier time-in-range. Programs typically reduce A1C by about 0.3–0.6% and can cut avoidable ER visits when paired with coaching and clear escalation paths.
If the app drives diagnosis/treatment, controls a device, or hides its rationale, it’s usually a regulated medical device and needs a 510(k) or De Novo, a quality system (QMSR/ISO 13485), and cybersecurity documentation. If it only supports clinician decision-making with transparent logic, it may qualify as Non-Device CDS. A short regulatory assessment early will confirm the path.
AI can flag risk from glucose trends, predict lows/highs, personalize nudges, and triage provider worklists. Keep models explainable, monitored, and human-in-the-loop; don’t automate dosing decisions without clearance.
Plan roughly 10–12 weeks for an MVP and pilot, 4–6 months to harden for production with EHR and reimbursement workflows, and 6–9 months for multi-device, multi-site scale. Complexity, integrations, and compliance scope drive the variance.









