Build an App for Your Chiropractor Clinic: Beyond Basic Booking
Planning to develop a chiropractic clinic app? Treat it like an operations upgrade, not a feature buffet. Clinics don’t lose to competitors—they leak at handoffs: intake to plan, plan to visit, visit to billing. Build the spine first (auth, audit, consent), then snap in the muscles: plan-aware reminders, state-aware telehealth, ABN flows for Medicare, after-hours booking, and cash-side inventory for orthotics and supplements.
Tie it to the only dashboards that matter—no-show rate, plan completion, days-in-AR—so you can prune what doesn’t move revenue. With Specode’s HIPAA-ready components, you assemble what works now and swap the rest later—no monoliths, no hero-coder mythology. Ship the machine that pays for itself, then get fancy.
Key Takeaways
- Ship the plumbing first—fast. Use a HIPAA-ready healthcare AI builder (Specode) to assemble the non-negotiables—auth, audit trails, e-consent, ABN—before features. You’ll get scheduling and EHR touchpoints wired quickly and avoid a rebuild later.
- Design for dual revenue models from day one. Support insurance-based acute care and cash-based maintenance/products in the same stack (pricing, documentation, scheduling, receipts).
- Run the clinic by the numbers. Track plan adherence, no-shows, note-closure time, and days-in-AR; ship changes that move those metrics next sprint.
The Untapped Digital Transformation in Chiropractic Care
Most chiropractor app development conversations start in the wrong place—with scheduling. But the real economics of modern chiropractic have shifted toward maintenance care models, where patient lifetime value beats one-off adjustments by multiples.

The problem? Your patients are dropping off before they get there.
Industry data shows practices retain only 40-60% of patients, with most abandoning care mid-treatment plans. That's revenue walking out the door because you're missing the digital touchpoints between visits.
The tech gap is glaring. Patients expect a digital health experience—93% according to recent HIMSS research—yet most practices run on paper handouts and voicemail. Meanwhile, according to the American Chiropractic Association, 40% of appointments get booked after hours when your office is closed.
Your patients are shopping for supplements on Amazon at 10 PM, tracking workouts on apps, but getting static photocopies for their rehab exercises. The disconnect isn't just inconvenient; it's expensive.
Industry veterans like ChiroFusion report the average practice loses $2,400 monthly from missed appointments alone, before counting the opportunity cost of lost maintenance plans.
The Revenue Reality of Digital Tools
Here's what happens when practices actually build an app for chiropractor workflows that extend beyond basic booking:
- Exercise compliance jumps from 30% to over 70% when patients get video guides, progress tracking, and in-app accountability versus paper handouts
- Patient retention increases 25%, with matching gains in referrals—turning your app into a practice growth engine
- Lifetime patient value extends as episodic care converts to maintenance relationships through continuous engagement
The global chiropractic software market—growing from $193.1 million to $239.6 million by 2030—tells you where smart money is moving. But generic practice management platforms miss the mark.
Real transformation requires chiropractic app design that creates a care loop: appointment scheduling flows into personalized exercise programs, patient management tracks progress between visits, and practice analytics show you which interventions drive retention.
Expert Perspective: "What patients are demanding these days is a digital health experience," says Dr. Jay Greenstein, DC, founder of Embodi and a board-certified physiotherapist who's spent decades transforming chiropractic economics through technology. "Features like remote therapeutic monitoring and gamification improve outcomes for our patients and also drive more income for providers." His peer-reviewed research on app-based rewards programs proved what forward-thinking practices already know: patient reviews improve when engagement deepens, and engagement deepens when care extends beyond office walls.
Chiropractic vs. General Healthcare Apps: Critical Differences
Most chiropractic mobile app failures start with the same assumption: "It's just another medical practice, right?" Wrong.
Chiropractors navigate a regulatory maze that makes general healthcare look straightforward—biomechanical documentation requirements that would baffle an orthopedist, insurance rules that treat Tuesday's adjustment differently from Thursday's, and scope boundaries that shift dramatically every time you cross a state line.
Biomechanical Assessment Requirements Unique to Chiropractic
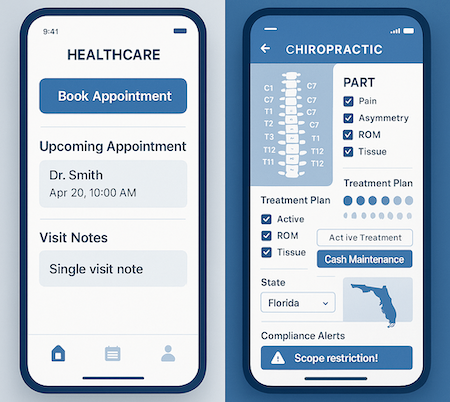
Generic EMRs choke on subluxation documentation because they weren't built for the PART framework (Pain, Asymmetry, Range of motion, Tissue tone) that insurance auditors demand. Your initial visit needs rock-solid proof of subluxation—whether through X-ray findings or at least two PART elements—plus the exact spinal levels you're adjusting.
Then every subsequent visit requires fresh documentation linking those same PART elements to the treated segments.
Smart chiro apps enforce this structure through templates, not free text boxes. They prompt for:
- Named spinal levels (not "mid-back")
- Measurable functional goals tied to subluxation
- Visit-by-visit progress tracking against initial findings
- Automatic flagging when documentation gets thin
Without these guardrails, you're building an audit magnet.
The Complex Dance Between Insurance-Covered Acute Care and Cash Maintenance
Here's what Medicare actually covers from chiropractors: manual spinal manipulation (CPT 98940-98942). That's it. No exams, no X-rays, no therapeutic modalities—just the adjustment itself. And even that comes with strings attached. You must prove "active treatment" with functional improvement, typically within 12 weeks for acute cases.
The moment care becomes maintenance—when the patient plateaus or shifts to wellness visits—Medicare stops paying. A properly designed mobile health app chiropractic system handles this transition automatically:
- Applies the AT modifier for active treatment claims
- Monitors progress metrics for plateau indicators
- Triggers ABN (Advance Beneficiary Notice) workflows when approaching maintenance
- Seamlessly flips billing to self-pay with proper GA modifiers
This isn't just about insurance verification; it's about building workflows that anticipate the acute-to-maintenance transition before it becomes a collections nightmare.
Multi-Visit Treatment Plans vs. Episodic Care Models
Unlike urgent care's "treat and street" model, chiropractic operates on treatment plans—structured progressions with defined frequencies, durations, and functional endpoints. Generic healthcare apps built for episodic visits completely miss this rhythm.
Your app needs to support care plan architectures that track:
- Initial treatment frequency (often 3x/week tapering to 1x/month)
- Re-exam triggers at specific intervals
- Progress benchmarks tied to functional improvements
- Automated reminders when plans approach expiration
Without these features, practices lose patients mid-treatment and leave money on the table.
Overlapping Scopes with PT, Massage, and Pain Management
"We also offer massage and acupuncture" sounds simple until you hit the regulatory wall. Some states prohibit chiropractors from employing PTs without physician ownership. Half the states bar DCs from performing acupuncture without separate licensure. Massage therapy usually requires an LMT unless performed incidentally within the chiropractic encounter.
Your payment processing and billing workflows must segment by provider type, with separate NPIs and service restrictions based on actual licensure—not what the front desk thinks is allowed. One wrong claim can trigger fraud investigations.
State-by-State Regulatory Variations That Break Generic Solutions
Scope variations are staggering. Oregon lets chiropractors sign birth certificates and perform minor surgery. Other states restrict them to spine-only adjustments. California mandates written AND verbal informed consent for spinal manipulation. Georgia requires 10-year retention for X-rays.
Virtual consultations? About 25 states explicitly allow tele-chiro, a dozen don't, and the rest exist in gray zones. Even where legal, coverage rarely follows. Apps must geofence services, display state-mandated Board notices, capture telehealth-specific consent, and restrict remote codes to consultation and exercise instruction—never manipulation.
The bottom line: if you want to create chiropractor application workflows that actually work, stop thinking "healthcare app with chiro branding." Think compliance engine with state-aware feature toggles, Medicare-proof documentation flows, and HIPAA compliance baked into every interaction—not bolted on after launch.
Technical Deep-Dive: Spine Assessment Integration
Most chiropractic apps stop at appointment booking, but the real clinical power lies in connecting your specialized assessment tools into a unified diagnostic ecosystem. The technical challenge isn't trivial—each system speaks its own language, and getting them to communicate requires more than wishful thinking and generic APIs.

Connecting PostureScreen, SEMG, and Thermal Imaging Systems
Integration complexity varies wildly across assessment tools, and understanding these differences determines your development timeline and budget.
PostureScreen operates as a one-way data push system. When an assessment completes, it fires off HTTP POST requests containing PDF reports and JPG images to your backend server. Here's the catch: there's no API to query historical data, and the system doesn't prevent duplicate submissions. Your backend must handle:
- Webhook endpoint configuration to catch incoming data
- Version control for duplicate submissions
- Patient record reconciliation without unique identifiers
- Storage optimization for multiple large image files per assessment
SEMG systems present the steepest integration cliff. Major manufacturers like MyoVision and Noraxon maintain closed ecosystems without public APIs. The only viable workaround involves building a custom middleware agent that:
- Monitors a designated "watch folder" on the clinic computer
- Parses exported CSV files or proprietary formats (.wst files)
- Uploads parsed data to your application backend
- Handles file naming conventions for patient matching
Thermal imaging offers the smoothest path via Teledyne FLIR's mobile SDK. Unlike the other systems, you can directly connect FLIR cameras to your spine analysis app, streaming live thermal video and accessing raw radiometric data.
This transforms your app from passive viewer to active analysis tool, calculating temperature differentials across specific vertebral segments in real-time.
Building 3D Spine Visualization That Actually Helps Treatment
Static X-ray viewers waste the diagnostic potential of digital imaging. To develop a chiropractic clinic app that actually improves clinical outcomes, you need multi-layered visualization that correlates structure with function.
The foundation starts with DICOM integration through your clinic's PACS server. Using mobile DICOM libraries like DICOMHERO, your posture assessment app retrieves X-ray data and constructs 3D models using rendering engines similar to OsiriX. But here's where it gets interesting:
- Thermal overlays: Map temperature data as color gradients directly onto the 3D spine model
- SEMG correlation: Display muscle firing patterns adjacent to specific vertebrae
- Postural vectors: Visualize force lines and weight distribution from PostureScreen data
- Time-based animation: Show progression between visits as animated transitions
This approach mirrors professional tools like PostureRay but brings the analysis directly to mobile devices, enabling tableside patient education during consultations.
Data Standardization Across Different Assessment Tools
Raw integration means nothing if your data remains siloed in incompatible formats. Your backend must act as a universal translator, converting diverse inputs into queryable, comparable datasets.
The chaos you're dealing with:
- PDFs and JPGs from PostureScreen
- Proprietary .wst files from MyoVision
- CSV exports from SEMG systems
- Raw radiometric arrays from FLIR
- Complex .dcm objects from PACS servers
The solution architecture: Build a patient-centric NoSQL data model where every input transforms into standardized JSON objects. Each assessment gets tagged with:
- Unique patient identifier
- Timestamp with timezone handling
- Assessment type and version
- Normalized measurement units
- Source system metadata
This standardization enables cross-modal analysis—comparing thermal inflammation patterns with SEMG hyperactivity and postural compensation patterns—creating insights impossible with standalone systems.
Creating Progress Tracking That Proves Efficacy to Insurers
Insurance reimbursement increasingly demands objective outcome metrics. Your spine assessment app must generate compelling visual and numerical evidence of improvement.
Effective progress tracking requires:
- Baseline establishment: Capture comprehensive initial assessments across all modalities
- Consistent intervals: Schedule reassessments at insurance-relevant milestones (2, 4, 8, 12 weeks)
- Automated comparisons: Generate side-by-side reports showing percentage improvements
- Clinical correlation: Link objective measurements to subjective pain scales and functional assessments
The output should mirror professional documentation systems like ChiroSight—presenting 15% reduction in forward head posture alongside corresponding decreases in trapezius hyperactivity and normalized thermal patterns. This multi-modal progress tracking transforms "patient feels better" into "quantifiable biomechanical restoration."
Mobile Capture vs. Clinic Equipment Integration Strategies
Your 3D spine analysis architecture must support two distinct data acquisition strategies, each with specific use cases and limitations.
Mobile capture leverages the device itself as the assessment tool—PostureScreen's camera-based analysis, FLIR ONE thermal attachments, or accelerometer-based range-of-motion testing. This approach offers portability and lower costs but limits assessment depth.
Clinic equipment integration connects to stationary diagnostic systems through network protocols or file-based workflows. While more complex to implement, it provides access to high-resolution X-rays, professional-grade SEMG arrays, and specialized biomechanical platforms.
The most successful implementations embrace both strategies, using mobile tools for routine posture monitoring while integrating clinic equipment for comprehensive evaluations. This hybrid approach ensures complete clinical documentation regardless of assessment location or available equipment.
The Dual-Model Architecture Challenge in Chiropractic Clinic Software
Most chiropractor app builder solutions assume you’re either insurance-based or cash-only. Real clinics run both: insurance for acute care, memberships for wellness, and cash packages for specialty work—while dodging dual-fee-schedule audits. Charging different rates by payment method creates legal and ethical risk.

The real headache isn’t “two payment types.” It’s enforcing shifting compliance boundaries while keeping UX clean. Your billing integration must auto-route treatment plans to the right pipeline—no staff tab-hopping.
Insurance Path Complexity
When a patient has Blue Cross, the system should trigger:
- real-time eligibility verification
- pre-authorization for certain codes
- documentation standards for medical necessity
- claims submission with proper modifiers
Miss a step and denials drag 45–60 days.
Cash Model Requirements
Cash doesn’t erase compliance. You still need HIPAA; the No Surprises Act requires good-faith estimates; time-of-service discounts typically cap at 5–15%. Consent forms need different language, the patient portal shows transparent pricing (not coverage), and receipts must itemize for HSA reimbursement.
The Smart-Routing Must-Haves
Your chiropractic billing app should:
- keep separate fee schedules without dual-pricing violations
- switch documentation rules by visit type
- track services per payment model for audit trails
- handle mixed visits where some services are covered and others aren’t
Without the right architecture, staff build shadow spreadsheets, compliance risk snowballs, and patients get confusing bills.
The answer: bake payment intelligence into every workflow—from booking through referral management. Every touchpoint should recognize payment context automatically. That’s the jump from a basic booking tool to a true chiropractic practice app.
Features That Actually Move the Needle
Most chiropractic apps stop at basic booking—yours shouldn't. The features that separate a mediocre app from one that transforms your practice all share one trait: they eliminate friction where it matters most.
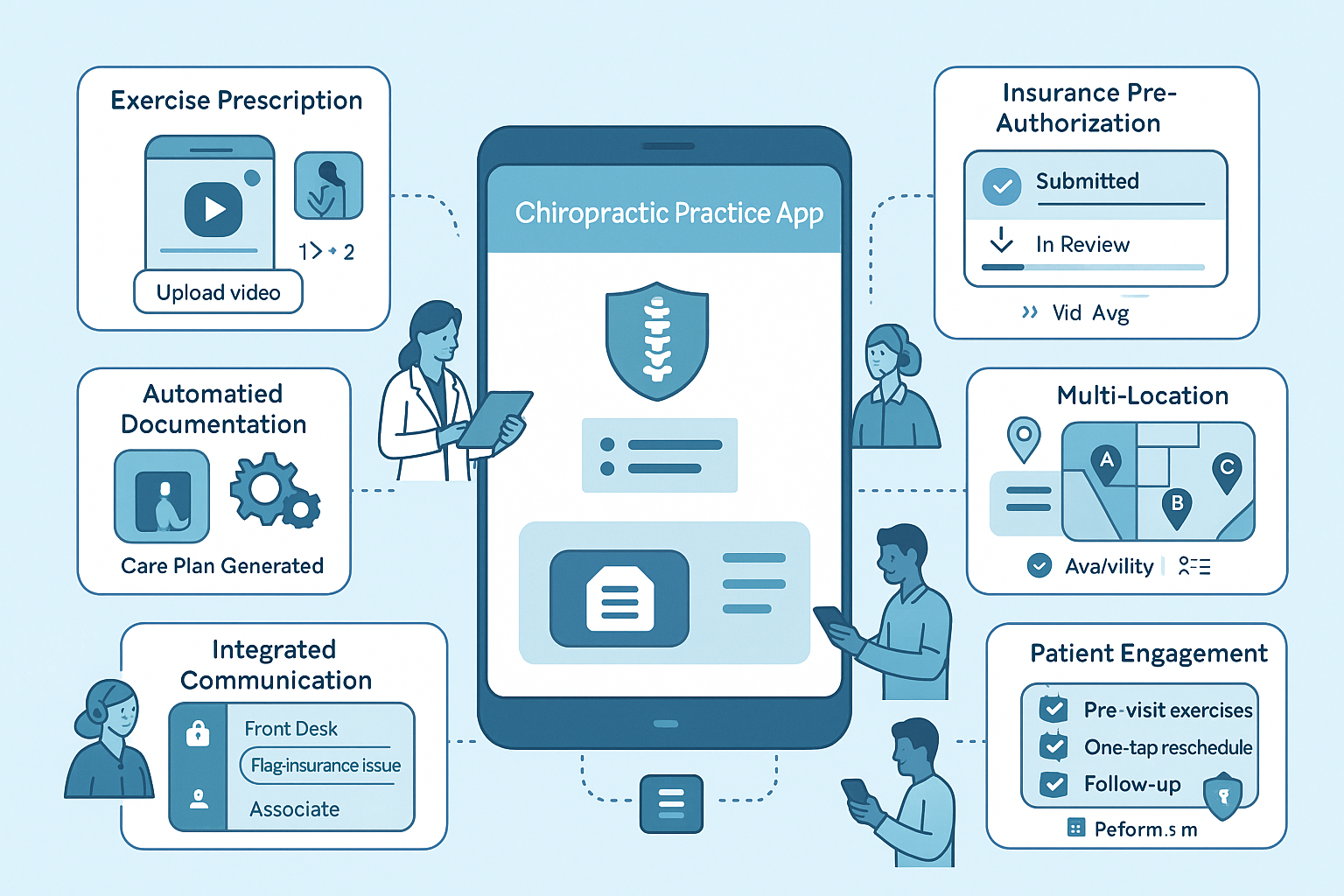
Exercise Prescription That Drives Compliance
Exercise prescription with form-check video analysis changes the game for patient compliance. Instead of handing out photocopied sheets that end up in glove compartments, your patient intake app chiropractor can push customized exercise videos directly to patients' phones.
The real magic:
- Video upload capability where patients record themselves doing exercises
- Asynchronous feedback from providers catches compensation patterns early
- Built-in accountability between visits
- Push notifications for exercise reminders
Automated Documentation That Saves Hours
Automated care plan generation based on assessment data cuts documentation time from 15 minutes to 2. Your initial evaluation populates treatment plans automatically—pulling from evidence-based protocols matched to specific conditions.
Key automation benefits:
- Visit frequency recommendations adjust based on chronicity and severity scores
- Insurance parameters automatically factored into care plans
- Patient records update across all providers instantly
- Less paperwork means more time for patient care
Insurance Pre-Authorization: The Real Time-Saver
Here's what actually moves the needle financially: insurance pre-authorization automation. UnitedHealthcare processes take an average of 4 business days, though members report waiting 8-10 days for approval.
When you build chiropractic mobile application features that auto-submit authorization requests immediately after evaluation, you're not just saving time—you're accelerating cash flow. The app should:
- Track authorization status in real-time
- Flag approaching visit limits before they expire
- Alert staff when coverage is running out
- Auto-populate required documentation
Patient Engagement Tools That Reduce No-Shows
Patient engagement tools tackle the expensive reality that no-shows account for 20.6% of missed appointments in chiropractic practices. But here's what works: automated reminder systems report a 29% reduction in no-shows.
Smart appointment reminders go beyond "See you tomorrow":
- Include pre-visit exercises in the reminder
- Provide parking instructions and office updates
- Enable one-tap rescheduling if conflicts arise
- Send follow-up messages post-treatment for feedback
Integrated Communication Beyond Basic Messaging
The chiropractic practice management app features that matter integrate real-time messaging for care coordination. Not just patient chat—but HIPAA-compliant team communication where:
- Front desk can flag insurance issues instantly
- Associates can request case consultations
- Everyone sees patient record updates in real-time
- Care teams coordinate without phone tag or sticky notes
Multi-Location Management Challenges
For growing practices with multiple locations, the challenges multiply:
The Problems:
- Maintaining consistent protocols across sites
- Sharing patient records between locations
- Coordinating provider coverage when staff floats
The Solution: Cloud-based architecture with role-based permissions where:
- Patients see availability across all locations in one view
- Records follow patients seamlessly between clinics
- Standardized workflows maintain quality while allowing location-specific customization
- Central dashboard tracks performance metrics across all sites
These aren't nice-to-haves. They're the features that reduce overhead, improve outcomes, and make your practice the one patients actually recommend.
Build vs. Buy: The Reality Check
Thinking about building a custom chiropractor appointment app from scratch? Here's the cold math that sends most single practices running:
- 31% of custom healthcare software projects get cancelled before completion
- another 52% blow past their budget by 189%

For a chiropractic clinic dreaming of digital transformation, those aren't just statistics—they're potential practice killers.
The fantasy of perfect customization crashes into three brutal realities. First, electronic health records integration alone can cost $30,000 to $200,000, with data migration eating up months of developer time. One format mismatch between your legacy system and the new build, and you're looking at weeks of additional cleanup work that wasn't in anyone's original estimate.
Second, the maintenance monster never sleeps. Plan on 15-25% of your initial development cost every year just to keep the lights on—security patches, OS updates, bug fixes, and the inevitable "the booking button stopped working on Android 15" emergencies.
For a $100,000 build (conservative for healthcare), that's $25,000 annually before you add a single new feature. Small practices typically lack the IT bandwidth to handle this ongoing burden, leading to security vulnerabilities and degraded performance over time.
The Hidden Complexity Tax
Patient intake forms seem simple until you factor in HIPAA compliance, conditional logic, document uploads, and signature capture across devices. What looks like a two-week sprint becomes a two-month slog once you add:
- Field validation that handles edge cases (international phone numbers, hyphenated names, insurance variations)
- Offline capability for spotty clinic WiFi
- Auto-save functionality to prevent data loss
- Integration with your practice management system
- Accessibility compliance for older patients
The integration maze gets worse with multi-location support. Suddenly you need location-specific scheduling rules, provider availability matrices, centralized reporting with location filtering, and inter-office patient record sharing. Each location multiplies complexity exponentially, not linearly.
When Custom Actually Makes Sense
Custom development works for three scenarios: multi-location practices with $5M+ revenue and dedicated IT staff, specialized clinics with truly unique workflows that no platform supports, or practices building proprietary technology as a competitive advantage (think franchise systems or teaching clinics developing their own protocols).
Even then, the smart money starts with proven components. A chiropractic telehealth app doesn't need custom video infrastructure—you need HIPAA-compliant video that works, integrated with scheduling and documentation. Building video calling from scratch when compliant SDKs exist is burning money for the sake of control.
The Component-Based Middle Path
The sustainable answer sits between off-the-shelf limitations and custom development hell: modular, HIPAA-ready components you can assemble and customize. Instead of coding authentication from scratch, you start with proven auth modules.
Rather than building patient scheduling, you configure existing booking components for chiropractic-specific needs (treatment series, multi-visit packages, recurring adjustments).
This approach cuts typical development time from months to weeks while maintaining code ownership. You're not locked into a SaaS platform's roadmap, but you're also not reinventing the wheel for every basic feature. When regulations change or you need that specific intake workflow for workers' comp cases, you can modify the components without rebuilding the entire system.
The verdict? Unless you're running multiple locations or have genuinely unique requirements that justify a six-figure investment and ongoing maintenance burden, the build-everything path leads to abandoned projects and blown budgets. The practices that thrive digitally are those that invest their customization budget where it matters—their unique care protocols and patient experience—not rebuilding infrastructure that already exists in battle-tested form.
Skip the heroic custom chiropractor app attempt. Use proven components where healthcare apps converge, then make your mark where your practice truly differs.
Implementation Roadmap for Smart Practices
You don’t need a moonshot; you need sequencing. Ship the boring-but-critical first, then layer insight.
Phase 1: Core operations and compliance
Goal: run a tight clinic day with audit trails.
What ships: intake & e-consent, chiropractor scheduling app (patient + front desk), secure messaging, payments, role-based access, PHI logging.
Checklists: HIPAA BAAs in place, retention windows, breach playbook, least-privilege roles, logging on every PHI read/write.
Call it: do not custom-build auth, audit, or consent—assemble from HIPAA-ready components and keep code ownership.
Phase 2: Assessment tool integration
Goal: make the exam quantifiable.
What ships: posture/spine assessment forms, image/X-ray attachment + role-gated viewing, templated SOAP notes, treatment-plan templates, inventory tracking for supplies you dispense.
Checklists: structured data models, e-sign on care plans, export mappings (PDF/CCD/CSV) ready for payers/referrers.
Call it: avoid a hard EHR dependency in v1—stub targets; add real integrations only when workflows stabilize. Partners for eRx/labs/wearables come later if truly needed.
By mid-build, your chiropractic patient app should already close the loop from intake → exam → plan → billing, with guardrails baked in—not bolted on.
Phase 3: Patient engagement and retention
Goal: reduce no-shows; increase plan adherence.
What ships: reminders, progress tracking, home-exercise videos, patient education library, review prompts, simple referral links.
Checklists: targeted notifications tied to plan milestones; staff management rules for who can nudge whom; clinic management dashboards for capacity; privacy-safe analytics on engagement.
Phase 4: Advanced analytics and optimization
Goal: spot bottlenecks and ROI levers.
What ships: dashboards for chair time, note-closure time, plan completion, payer mix, days-in-AR; cohort views by condition/provider; anomaly alerts.
Checklists: immutable audit queries, export to BI, North-star KPIs that the team actually reviews weekly.
Call it: if a metric won’t change a decision next sprint, don’t instrument it.
Realistic timelines and resource requirements
(Assuming a component-assembly approach vs. from-scratch.)
- Weeks 1–2 (Phase 1): requirements, component mapping, compliance baseline; PM/architect, 1–2 engineers, designer, part-time compliance.
- Weeks 3–4 (Phase 2): assessments, plans, exports, “fake EHR” stubs; same team; clinician reviewer on call.
- Weeks 4–6 (Phase 3): engagement flows, education, review mechanics; add content ops for patient education.
- Weeks 6–8+ (Phase 4): analytics, BI extracts, tuning; data engineer/analyst as needed.
Teams using reusable HIPAA-compliant components routinely hit a 6–8 week MVP/V1, then iterate without platform lock-in.
Sanity checks before you start: if any vendor can’t sign a BAA, pass. If an integration doesn’t move a KPI in the next quarter, defer. If “inventory tracking” exists only in someone’s spreadsheet, formalize it now—or your dashboards will lie later.
How Specode Helps Chiropractic Tech Innovators
If you’re building a mobile app for chiropractors, Specode gives you the fast lane without the lock-in.

Pre-built HIPAA Components for Dual-Model Practices
Run insurance-covered acute care and cash-based maintenance on one stack. Assemble: auth & roles, intake/e-consent, chiropractor booking app scheduling, telehealth, secure chat, notifications, goals/symptom tracking, “Resources” for patient education, basic or advanced EMR, and payments/claims.
AI Assistant: Build by Chat, See It Live
Describe the chiropractic flow—new-patient vs maintenance intake, plan-of-care scheduling, SOAP-style notes, outcome tracking—and watch it assemble with an instant preview. Connect your own data early so screens and rules reflect real patients, providers, and codes—not mockups.
Start on a healthcare foundation (roles, consent, audit), then toggle only what matters for your clinic. When something is truly unique, drop into code—or tap our Custom tier for managed help or purpose-built AI agents. No AI magic—sequence and ruthless focus.
- Prompt → preview: update fields, branching, and validations in seconds.
- Integration switchboard: payments, telehealth, wearables/EHR, and insurance rails stitched into your flows.
- Guardrails: Change Log restore and role-scoped testing keep experiments safe.
- Fully brandable: logo, colors, and typography from day one.
Proof > Pitch: Real-World Wins
- AlgoRX: medication storefront built from assembled components—eligibility, provider workflow automation, multi-pharmacy routing—hit $1M+ by month 2 and 12× ROI within months.
- DyadSync: streamlined clinician scheduling, payments, and messaging for surgical teams—proof that composable scheduling + comms untangles real-world ops quickly.
Why Component Assembly Beats Custom for Specialized Clinics
- Compliance by construction: HIPAA-aware modules with audit trails and least-privilege roles from day one—no “retrofit security” tax.
- Own the code, avoid platform ceilings: extensible components you can keep evolving post-launch.
- Scope honestly: start with scheduling, intake, telehealth, and messaging; add wearables or symptom tracking for pain management when it actually changes outcomes.
Clear Path from MVP to Scale
- Weeks 1–8: requirements → component mapping → assembly → QA → go-live, with explicit EHR/eRx/labs handled via partner integrations when needed.
- Operational depth: clinic management dashboards, staff management via roles/credentialing, [Inference] basic inventory tracking repurposed from the product catalog to keep supplies honest, and a patient education library that actually gets used.
If you’re deciding between rebuilding the plumbing or shipping outcomes, Specode’s assembly model is the pragmatic path—from “book, examine, document, charge” MVP to durable chiropractic clinic software.
Start free on Specode—add intake + ABN consent, brand your booking page, and preview in minutes; then layer cash packages and insurer visits and run a one-week front-desk pilot.
Frequently asked questions
Assemble HIPAA-ready components (auth, intake/e-consent, scheduling, messaging, payments) and defer hard EHR work until workflows stabilize.
Encode rules: AT/GA modifiers, ABN prompts, plateau detection, and automatic routing to self-pay when active treatment ends.
No. Use compliant SDKs integrated with plan milestones and documentation; build value around workflows, not media servers.
No-show rate, plan completion %, days-in-AR, note-closure time, review velocity. If a metric won’t change a decision, don’t instrument it.
Plan-aware reminders, exercise videos with async feedback, and progress visualizations tied to visit cadence.
Centralized protocols with location overrides, shared records, role-based staff management, and inventory controls per site.
Buy/assemble the commodity pieces; invest custom effort where your protocols differ (treatment plans, insurer rules, education).









